A boil on the penis is a serious problem that brings a man a lot of pain and discomfort. Boil (common name) is characterized by an acute purulent inflammatory process of connective tissue and hair follicle.
The disease is caused by white or aureus staphylococcus. An abscess can begin to develop at any age, but is most often observed in young men.
What causes ulcers on the penis
An abscess on the body is also called a boil.
This rash is characterized by an inflammation process.
It develops most often in the area where hair grows.
Pustules can form at the location of the sebaceous glands or connective tissues.
The cause of the appearance of pustules on the penis is damage to the organ by pathogenic microorganisms.
They provoke the development of the inflammatory process.
The most common causative bacteria is Staphylococcus aureus or white Staphylococcus.
There are several types of pustules on the penis:
- recurrent
- single
- multiple
Recurrent pustules may appear intermittently.
They develop in several stages.
Let's look at each separately.
The first is called infiltration.
At this stage, the formation of a pustular lesion begins.
This is the stage of formation of an abscess.
An element of a rash appears, inside it contains liquid with pus.
Rejection is characterized by opening and draining of pus from the mass.
After all the pus is released, the scarring stage begins.
The wound is healing.
Subsequently, a scar may remain in this place.
It should be noted!
If an abscess appears on the penis, you need to consult a specialist.
Self-medication can cause secondary infection in the wound.
Sometimes it is quite difficult to determine the exact cause of the formation of an abscess on the genital organ.
Most often, the examination reveals several factors.
The following are distinguished:
- decreased immune system function
- diseases of the gastrointestinal tract
- abuse of alcohol and tobacco products
- presence of microtraumas
- wearing poor quality, tight underwear
- poor personal hygiene
- hormonal imbalances
- frequent stress
- lack of vitamins in the body
If the above symptoms are present, pustules may appear on the penis.
Various diseases can also affect the formation of rashes in the intimate area.
Let's talk about them in more detail.
Stages of development of furunculosis
The disease occurs in several stages. The ideal start for starting treatment is the first period.
- Infiltration stage . The appearance of an abscess is preceded by itching and redness; later, a feeling of pain and tingling occurs at this site. The purulent infiltrate gradually covers the entire hair follicle and adjacent tissues. Swelling may be noticeable on the skin.
- Stage of suppuration. Gradually the pain intensifies and causes severe discomfort when moving. After 3-4 days, a fluctuation zone is formed. Inside the boil, movement of purulent masses is felt, and a fistula forms on the surface.
- Resolution stage. When an abscess is opened, thick pus is released, sometimes mixed with blood. At the bottom of the abscess you can see a small greenish rod. It leaves afterwards along with pus and blood.
- Healing stage. After the boil resolves, the pain goes away. Small abscesses do not leave ulcers upon opening.
Volumetric ulcers, after the contents are released, leave ulcers with a deepening into the skin. Then a scar often remains at the site of wound healing.
Ulcers on the penis due to furunculosis
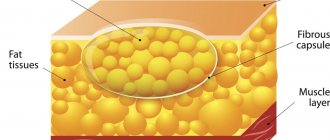
A purulent abscess is called a boil.
It can form on absolutely any part of the body.
The penis is no exception.
External and internal factors have a direct impact on the formation of boils.
External factors:
- bad ecology;
- failure to comply with intimate hygiene rules;
- genital hair removal;
- use of linen made from synthetic fabrics;
- local overheating or hypothermia.
Internal factors:
- weakened immunity;
- hormonal imbalance;
- presence of diabetes mellitus.
The development of a boil occurs in stages.
First, a small lump forms on the penis.
At the first stage, the surface of the formation is hyperemic and has a higher temperature.
This indicates that the sebaceous gland is blocked.
A critical amount of sebum has not yet accumulated in the omentum.
At this stage it is easiest to get rid of the boil.
The second stage is characterized by the formation of a white purulent core inside the boil.
This occurs due to a large accumulation of subcutaneous fat inside.
The head of the boil is located at the end of the rod.
The formation at this stage of development must be opened surgically.
Independent opening of the boil is typical for the third stage.
Separation of purulent contents occurs along the walls of the shaft of the boil itself.
The rod itself remains inside.
To remove it, washes with antiseptic liquids are carried out.
Complications do occur.
One of them is septic damage to the dermis.
It develops when the pathological contents of the boil are separated into the inner layers of the patient’s dermis.
This problem can only be treated surgically.
Diagnostics
To determine an accurate diagnosis of the reason why his genitals are strewn with ulcers, the patient is prescribed a number of diagnostic measures:
- visual inspection;
- taking anamnesis;
- study of biological material of ulcers and tissues from their walls;
- urethral smear;
- general and biochemical blood test for the presence of sexually transmitted diseases;
- urine examination, bacteriological culture (when examining blood fluid, PCR and ELISA methods are used);
- Ultrasound of the penis;
- lymph node biopsy;
- MRI or CT.
Modern diagnostics guarantees successful treatment of the resulting pathology.
Ulcers on the penis due to herpes
Herpes is a common, highly contagious viral disease.
There are many types of virus.
Genital herpes is one of the most common.
The virus is transmitted through unprotected sexual intercourse.
Oral and anal contact are also factors in the transmission of the disease.
A household method of transmission is also possible.
Small blisters appear on the head of the penis, in the perineum or on the scrotum.
They are filled with liquid.
The process is accompanied by itching.
After some time, the watery blisters begin to burst.
In their place, ulcers form and are covered with scabs.
In some cases, blisters may appear in the urethra.
This disease will be classified as herpetic inflammation of the urethra.
The first symptoms of herpes development can be confused with acute respiratory infections.
The patient is concerned about general lethargy and malaise.
Increased body temperature, discomfort and soreness in muscles and joints are acceptable.
A specific symptom is the formation of watery blisters on the penis. Urination is accompanied by a strong burning sensation.
A prolonged herpes virus infection can affect a man’s potency and reproductive functions!
Abscesses on the penis due to the immunodeficiency virus
HIV may not make itself felt for long periods of time.
Regular testing is very important for early diagnosis of the disease.
Suspicions about the presence of the disease can be caused by a skin rash, the formation of ulcers, and dermatitis.
In the case of HIV, these pathologies are not considered a separate lesion.
They act as opportunistic diseases.
That is why they are very difficult to treat.
The immunodeficiency virus causes skin lesions such as:
- Fungal infections. Rashes of various types are provoked by massive fungal proliferation.
- Pyoderma. Caused by streptococcal and staphylococcal infections.
- Manifested by the formation of ulcers with liquid contents.
- Spotted rash. The formation of red spots of varying sizes on the skin is characteristic and is caused by vascular disorders.
- Papular rash. It is characterized by the formation of a cluster of papules of various sizes.
What tests should be taken for an abscess on the penis?
To make the correct diagnosis and select the optimal treatment, you need to contact a dermatovenerologist!
The patient needs to undergo a series of diagnostic tests.
To diagnose furunculosis, fluid is taken from the abscess.
The pathological contents are placed on a nutrient medium where microorganisms can multiply productively.
The specialist identifies the pathogen.
Next, tests are carried out for sensitivity to antibacterial agents.
This will help you decide on a drug for further treatment.
To diagnose herpes, it is necessary to take a smear from the surface of the lesion.
The material is examined for the presence of pathogen DNA using the polymerase chain reaction (PCR).
The patient's blood serum is examined using the enzyme immunoassay method.
This is done to detect specific IgM and IgG antibodies.
To diagnose infection with the human immunodeficiency virus, an enzyme-linked immunosorbent assay is performed.
Its purpose is to detect antibodies.
Other laboratory tests may be necessary at the discretion of the attending physician.
Important!
Only high-quality diagnostics will help you choose the most effective treatment regimen.
Treatment methods for boils in the groin in men
To determine the method of recovery for the patient, the doctor must diagnose the body. You can seek help from a therapist or endocrinologist. The therapeutic option closely correlates with the degree of the disease and the personal characteristics of a person’s health. The following recovery methods are distinguished:
- medicinal. The use of antibiotics and antimicrobials has a healing effect. Doxycycline is popular. The duration of medication treatment reaches 10 days. An alternative option is Ciprofloxacin. The medicine qualitatively eliminates pathogenic microflora within a week. The daily dose of the substance is 2 mg. The perineum should be treated comprehensively;
- surgical. If a boil in the groin in men affects a large area, surgery will be inevitable. The patient is given pain relief with Ledocoin. The surgeon makes an incision so that the contents of the boil come out. Disinfection of the wound is carried out with a solution of Furacilin. A tourniquet is used as drainage;
- ethnoscience. In the first stages of the development of the disease, it is allowed to treat the inflamed area with an infusion of oak bark and chamomile. The antiseptic effect will stop the growth from growing. Next, an elixir of green plantain leaves is used. Pre-rinse and grind the ingredient to small particles. Gauze is soaked in the liquid and applied to the boil. Aloe and agave are used in the same way.
After the pus comes out, treat the wound with hydrogen peroxide. The disinfectant thoroughly cleans the wound and eliminates the spread of infection. The procedure is performed every 8 hours until the abscess is completely healed. The procedure should be stopped until a hard crust forms at the site of the removed chiryak.
Abscesses on the penis with molluscum contagiosum
Molluscum contagiosum develops as a result of the penetration of a virus.
It appears in the form of pustules on the head of the penis.
The nodules are dense and have depressions in the center.
This disease is transmitted through contact or sexual contact.
This disease does not pose any particular danger.
The incubation period for the appearance of molluscum contagiosum may vary.
Important!
From the moment of penetration to the first symptoms it usually takes from two weeks to six months.
At the end of the asymptomatic period, the active stage of the disease begins.
During this period, seals appear on the skin of the penis.
The nodules have a spherical shape.
Their sizes are quite small - up to 10 millimeters.
In rare cases, they can merge and form large plaques up to five centimeters.
Ulcers with molluscum contagiosum are white with a pearlescent tint.
The elements are dense and shiny.
When you press on the abscess, a white pulp will come out.
Formations can be either single or numerous.
Most often, ulcers appear in the groin area and armpit area.
Sometimes found on the stomach and face.
Rarely the mouth, feet and scalp are affected.
Ulcers on the penis due to scabies
Scabies is a skin disease.
Appears as a result of infection by parasites.
The causative agent of this disease is the scabies mite.
This disease can appear in various parts of the body.
The genitals are no exception.
When scabies appears in the groin area, it is necessary to conduct a series of studies.
This is necessary to accurately diagnose and eliminate the cause of the pathological process.
The first sign of scabies in the groin is severe itching of the skin.
Subsequently, pinpoint rashes form.
They are usually noted at the site of tick penetration.
Most often the glans and foreskin of the penis are affected.
During the active period of the disease, rashes appear on the scrotum and pubis.
A papular rash forms.
Ulcers are localized under the head of the penis.
The most common symptoms of scabies in the groin include:
- itchy sensations on the skin;
- small rash;
- burning sensation in the groin;
- hyperemia of the skin on the genitals;
- white stripes are the passages of parasite penetration.
If such symptoms are present, treatment should be started immediately.
Folliculitis: predisposing factors
Most of the listed pathogens rarely cause folliculitis, even if they come into contact with the skin of the penis.
Infection is not enough for the disease to develop.
Predisposing factors are also needed.
Only if for some reason the body cannot “repel” these pathogens, or very favorable conditions are created for their reproduction, does the pathological process begin.
As we have already said, most penile folliculitis is caused by staphylococcus.
While other forms of the disease often have no clinical significance (they go away on their own), or develop as a secondary manifestation of an existing pathology.
The main predisposing factors for the development of bacterial folliculitis:
- lack of adequate hygiene - cells and sebum accumulate on the skin, which are a nutrient substrate for bacteria
- increased level of androgens - sebum production increases, it mixes with exfoliated cells and clogs the mouth of the follicles
- microtraumatization is inevitable for men who remove hair in the intimate area, regardless of the method used (shaving, hair removal)
- excessive sweating – bacteria like to grow in a humid environment, so folliculitis often develops when wearing tight clothes, in hot and humid climates, and with a sedentary lifestyle
- fever – increases sweat production, and also creates favorable temperature conditions for some bacteria
- immunodeficiency states - in this case, purulent processes and infectious diseases attack a person from all sides, as the body’s resistance to bacteria, fungi and viruses decreases
- diabetes mellitus - carbohydrate metabolism disorders lead to vascular damage, metabolism suffers, microcirculation is disrupted, local immunity suffers
- local use of glucocorticoids - used mainly to treat local manifestations of allergies, although patients often use hormonal ointments for self-medication (including long-term courses), and this results in infectious inflammation of the skin
- taking immunosuppressants (for example, after an internal organ transplant)
Folliculitis develops more often in people with oily skin.
It is more often detected in male patients.
On the other hand, an important condition for the development of the disease is also the contact of bacteria with the skin of the intimate area.
They can get there in various ways:
- staphylococcus is often brought in by hand from one’s own nasopharynx, and is also always present in small quantities on the skin
- E. coli lives nearby, in the intestines
- candida fungus can be contracted through sexual contact
- This is where the herpes virus comes from
- dermatophytosis is initially present on the feet, but then the patient introduces fungi into the groin with unwashed hands, which results in skin lesions and folliculitis of fungal etiology
- All people have the Pityrosporum fungus, especially those whose sebaceous glands produce a lot of secretions (the main risk factor for folliculitis of the corresponding etiology is seborrhea)
- Pseudomonas infection often occurs through water
- syphilis is sexually transmitted, but folliculitis develops only several months after infection, against the background of other skin manifestations of syphilitic infection
Read also: Drips from the penis
Ingrown hairs are often a predisposing factor.
This is a condition in which the loose ends of the hair penetrate the skin.
Here a focus of inflammation is formed, to which bacteria (including staphylococci) often join.