Causes of exacerbation of psoriasis
For the first time, psoriatic rashes may appear at the age of about 15-25 years. It is impossible to completely cure the pathology. The main goal of therapy is to achieve long-term remission. Under the influence of provoking factors, an exacerbation of psoriasis may develop. This condition occurs due to the influence of the main root causes of skin pathology on the body, such as:
- long-term physical activity;
- overstrain of the nervous system;
- endocrine pathologies;
- contact with aggressive chemical compounds;
- the course of chronic inflammatory processes;
- autoimmune pathological conditions;
- infectious infection;
- drinking alcohol and smoking;
- influence of negative production factors;
- unbalanced diet;
- the influence of household products on the skin;
- long-term use of antibiotics, immunomodulators;
- grafting.
According to the seasonal development of exacerbations of psoriasis, there are forms of the disease:
- winter;
- summer;
- off-season.
In the chronic development of the disease, it is desirable to limit the influence of sudden changes in climatic conditions, since they can act as provocateurs of relapse. This factor is especially important when planning travel.
How to prevent a relapse
The easiest way is to prevent the development of an exacerbation of the disease, and this can really be done at home, without special procedures and drugs. Measures to prevent relapse are very simple:
- you need to protect yourself from stress. It is unlikely that it will be possible to do this fully, but it is quite possible to reduce their impact on the nervous system;
- carefully monitor your own menu;
- keep microflora under control;
- support immunity with vitamins.
Advice! Treatment of psoriasis cannot be called complicated; the main thing is to carefully monitor nutrition and other provoking factors, because the patient’s quality of life depends on this.
Main causes and provoking factors of relapse
The main reasons that provoke exacerbations of psoriasis are:
- Wrong diet. For psoriasis, it is advisable to control the intake of vitamins and mineral complexes. Since the lack of a balanced diet provokes a decrease in the body’s protective properties, which manifests itself through a relapse of psoriasis.
- Hormonal surges. Failures of this nature are observed while taking hormonal-based drugs and pathologies in the endocrine system. An imbalance in hormone levels occurs during pregnancy.
- Skin damage. In addition to mechanical scratches or wounds, chemical burns are also possible when using household chemicals.
- Emotional stress. The nervous system controls almost all processes in the body. Failures in its functionality lead to the development of exacerbations of chronic pathologies, and psoriasis is no exception.
- Medicines. There is an exacerbation of psoriasis due to prolonged use of antibiotics or immunomodulators.
- Genetic predisposition to autoimmune diseases.
Exacerbation of psoriasis may be caused by changing weather conditions, since the progression of pathology is often recorded in the winter.
Healthy eating and vitamin therapy
Nutrition in psoriasis plays an important role, since the frequency of relapses of the disease greatly depends on it.
Diet is expected; Here's what you can eat:
- dietary meat - rabbit, turkey, veal, chicken;
- white sea fish;
- vegetables and fruits that do not have too strong a taste or smell - apples, pears, bananas, cabbage, carrots.
Food needs to be steamed, baked or boiled. Fruits and vegetables can also be eaten raw.
The following products are excluded:
- tomatoes, peppers, potatoes;
- pork, lamb;
- high-percentage cheese and cream;
- sweets;
- butter;
- alcohol;
- nuts;
- citrus.
Attention! Semi-finished products, even from permitted products, are not acceptable.
In addition to a healthy diet, a patient with psoriasis should take pharmaceutical vitamins necessary for skin health and immune support.
We offer you to watch a video about proper nutrition during an exacerbation of psoriasis:
Risk factors
In summer and spring, there is a decrease in the possibility of exacerbation of psoriasis. And the autumn-winter period of time, on the contrary, is characterized by an increase in the area affected by the skin rash. The progression of pathology during periods of changing climatic conditions is determined by the influence of a complex of factors:
- Winter period. The main factor that provokes psoriasis is insufficient sun exposure. Friction of clothing against the skin reduces its protective properties. Dry air during the heating season leads to dehydration of the skin.
- Autumn. Provoking causes of relapse of skin pathology at this time include favorable conditions for infectious pathogens and decreased immunity.
- Summer period. The skin receives air baths, which have a beneficial effect on its protective properties. This time is characterized by a sufficient amount of ultraviolet radiation. It also needs to be monitored, since increased exposure to radiation can trigger the development of a psoriatic rash.
- Spring. At this time, psoriasis can be triggered by an allergic reaction to flowering plants.
Also, associated risk factors for the development of relapse of psoriasis include age, hypothermia, chronic pathologies and harmful habits.
Why does the disease worsen in winter and summer?
Often, the disease manifests itself during the cold season, since during this period a person’s immunity is vulnerable. In winter, harmful microorganisms are most active, so they are more likely to attack a weak body. Sun rays have a positive effect on the epidermis, but excessive amounts of ultraviolet radiation, especially in summer, provoke the formation of plaques on the skin.
Symptoms and clinical manifestations
Symptomatically, exacerbation of psoriasis is characterized by the appearance of new areas of rash. You may also experience:
- formation of papules and plaques on the skin;
- due to the removal of scales, a terminal film appears;
- damage to the skin of new areas of rashes is provoked by mechanical irritants;
- the pathology is accompanied by a strong feeling of scratching;
- hyperemia and areas of peeling with a clear limitation are formed;
- possible feeling of tight skin;
- scales form on the skin and peel off;
- compaction is possible in the affected areas;
- Sometimes cracks appear as a result of dehydration of areas of the skin.
The rash appears in the hair area of the scalp, palms, or soles of the feet. The danger is an exacerbation of psoriasis observed in females during pregnancy, because this pathology can provoke spontaneous abortion.
Physiotherapy
Physiotherapy is indicated after exacerbations of psoriasis have subsided. The procedures are carried out in spa treatment conditions and at specialized clinics and include:
- hydrotherapy with pine-salt baths,
- exposure to ultraviolet light,
- photochemotherapy (PUVA),
- cryosauna,
- hirudotherapy,
- electrosleep,
- pulsed phototherapy,
- impact by acoustic waves.
Climatotherapy is indicated for all patients in spring and autumn. The solar spectrum and sea salts eliminate the effects of psoriasis and have a beneficial effect on the duration of remission.
Exacerbation during pregnancy
A hormonal surge during pregnancy causes an exacerbation of psoriasis. The generalized course of pathology during pregnancy is provoked not only by hormonal changes, but also by a lack of vitamin D. Symptoms of the disease can be varied, somewhat similar to the symptoms of allergic manifestations. During exacerbation of psoriasis, certain symptoms are recorded in the form of:
- a large area of rash with the presence of reddened plaques, often in various parts of the groin or abdomen;
- after a while a feeling of pain and itching appears;
- the temperature may rise;
- attacks of nausea and vomiting are observed;
- There is no appetite at all.
A provoking aspect of exacerbation of the disease is an increase in the level of cortisol in the bloodstream of a pregnant woman.
Methods for relieving exacerbations
Diseases of the dermis can be dealt with using a systemic, comprehensive approach.
Methods to help relieve symptoms include:
- drug treatment,
- physiotherapy,
- dietary correction and healthy lifestyle,
- therapy with traditional recipes.
The dermatologist decides how to treat the disease, taking into account the stage of the disease, the nature of the rash and the general condition. Persistent remission is expressed in a reduction in the area of rashes and restoration of the skin.
How long does a psoriasis flare-up last?
It is impossible to achieve complete recovery of psoriasis. Therefore, the disease occurs in three stages:
- progression;
- stationary;
- regressive.
The first stage is characterized by the appearance of rashes, often at the site of injured skin. After a month, psoriasis may enter a stationary stage, during which silvery scales appear. The regressive stage can last about several months, during which the symptoms disappear. However, under the influence of provoking factors, exacerbation of psoriasis develops. No one can accurately determine the duration of the stage. To reduce the duration of an exacerbation, the patient’s main task is to follow therapy, diet and all the dermatologist’s prescriptions.
How to stop the development of pathology without hormones
All non-hormonal drugs are used in the initial stages of the disease.
Effective means that fight the visible symptoms of lichen planus - plaques - are ointments and creams using medical grease. Preparations for external use are divided into 3 groups:
- plant-based (“Antipsor”, “Akrustal”, “Kartalin”);
- on mineral substances (Rybakov ointment);
- combined (“Magnipsor”, “Cytopsor”).
Doctors also recommend using salicylic and zinc ointments, Daivonex, Losterin, Zinocap, Psoriaten.
What to do if psoriasis worsens
It is possible to relieve the symptomatic discomfort of exacerbation of psoriasis through complex therapy, which is contained in:
- Treatment with medications. Severe exacerbation of psoriasis is stopped through drug therapy. It often includes the prescription of sedatives, antihistamines and immunomodulators. If necessary, non-steroidal anti-inflammatory drugs can be taken. When prescribing treatment, it is mandatory to take vitamin and mineral complexes.
- Local ointments. To achieve remission, salicylic ointment or Kartalin is prescribed. These medications are characterized by anti-inflammatory and antibacterial properties. In case of exacerbation of psoriasis spreading to the skin under the hair, Sulsena or Ketazoral shampoos will help.
- Physiotherapeutic activities. The use of this technique in severe forms of skin pathology is justified. Common procedures include ultraviolet irradiation, hydrotherapy, and plasmapheresis.
When treating psoriatic rashes in the progression phase, it is better to stick to a diet.
Drug treatment
Medicines for the treatment of exacerbation of psoriasis have certain characteristics:
- relieve inflammation in the affected area;
- eliminate emotional stress;
- produce an antiallergic effect;
- strengthen the immunological status of the body.
Often the active ingredient in topical medications is:
- zinc compounds;
- salicylic acid;
- tar;
- solid oil
During exacerbation of psoriasis, topical medications are mandatory, since they directly affect the affected area. Effective drugs to combat skin pathologies are presented in the table.
| Drugs | Impact |
| Celestoderm | Relieves the severity of symptomatic manifestations. It is necessary to apply about 2 times in the morning and evening. |
| Elokom | The ointment is intended to eliminate psoriasis in areas with delicate and delicate skin. One application per 24 hours is sufficient. |
| Dovonex | Combats itching and hyperemia. The drug belongs to anti-inflammatory drugs. Use once within 24 hours. |
| Salicylic ointment | Moisturizes and soothes the skin, has an anti-inflammatory effect. |
Among the sedative medications during periods of exacerbation of psoriasis, the following are used:
- Novo-grazing.
- Valerian.
- Phytosed.
- Motherwort tincture.
To eliminate itching and hyperemia in the area of psoriatic rash, medications are used:
- Claritin.
- Diazolin.
- Suprastin.
To improve the functioning of the gastrointestinal tract and reduce intoxication, sorbents are prescribed:
- Smecta.
- Activated carbon.
- Sorbex.
Fish oil and folic acid are prescribed to the patient to improve immunity, which plays a major role in recovery.
Hungarian scheme
The main effect of bile acid is based on the limited entry of toxins of various etiologies into the body. The Hungarian scheme in case of exacerbation of psoriasis consists of intoxication through the use of an active component based on a bile substance - dehydrocholic acid. This active ingredient helps:
- removal of bile;
- formation of bile acids;
- normalization of glucose levels;
- increasing blood circulation in the liver tissues.
Diet during exacerbation
An individually selected balanced diet with useful minerals and a vitamin complex can eliminate the progression of psoriasis. With the development of chronic forms of the disease, it is imperative to adhere to a diet. During exacerbation of psoriasis, a positive effect is observed in case of fasting, namely the presence of fasting days. The essence of this technique is to use 1 product for 1 or 2 days. During this period of time, you should also avoid overeating, since then the patient’s condition may change for the worse. For preventive measures of exacerbation of skin pathology, 1 fasting day during the week is enough.
Physiotherapy
Therapy for diagnosing exacerbation of psoriasis also includes physiotherapeutic techniques. This method enhances the drug effect. The most common methods are:
- PUVA therapy;
- electrosleep;
- X-ray therapy;
- laser therapy;
- cryotherapy.
Thanks to physiotherapeutic manipulations, it is possible to achieve remission of psoriasis for about 3 years. Magnetic therapy and diadynamic therapy are effective methods for diagnosing psoriatic arthritis. Physiotherapy often takes place within the walls of a hospital. The duration of physiotherapy is about 12 sessions.
Which doctor should I contact during an exacerbation?
During an exacerbation, you need to contact a dermatologist directly. There are not always highly specialized doctors in all hospitals, so if such a doctor is not available, you need to go to a therapist.
Squamous lichen not only affects the skin, but can affect internal organs and the musculoskeletal system. Based on the patient’s complaints, a therapist or dermatologist may prescribe additional examinations with specialists such as:
- immunologist (with a significant decrease in the body’s defenses);
- rheumatologist (joint damage);
- urologist, nephrologist (kidney pathologies);
- gastroenterologist (liver diseases).
These specialized doctors help in the complex treatment of the disease. The main therapy is prescribed by a dermatologist based on the characteristics and causes of relapse.
If the disease worsens, consult a dermatologist
How to relieve an exacerbation of psoriasis at home
Traditional medicine acts as an auxiliary method in the fight against the progression of exacerbation of psoriasis. You can quickly relieve symptoms such as hyperemia and dry skin by using certain traditional medicine techniques. There are several effective recipes for this:
- Butter and propolis. To obtain the ointment, you need to mix 0.5 kg of butter and 50 g of propolis in a saucepan. The container is placed on the fire and the mixture is cooked until it becomes soft. After cooling, add 2 tbsp to the resulting ointment. l. sea buckthorn oils. The resulting medicine is applied 6 times throughout the day. To obtain a positive effect, about 8 sessions are required.
- Onion based compress. The onion can be chopped with a blender or knife. A compress is made from the resulting porridge on the affected areas. After several sessions, there is a decrease in the inflammatory process, softening of thickenings and increased regeneration processes of the skin.
- Baths. To eliminate the symptomatic manifestations of exacerbations of psoriasis, taking a bath based on aloe, celandine, and calamus root helps.
- Salt. To eliminate a strong feeling of itching, taking baths with sea salt is effective. To obtain the required solution, you need to dissolve 1 kg in a bath and swim for 15-20 minutes. After such baths, the main thing is to wash off the salt under running water.
Birch tar ointment
To obtain an ointment based on birch tar, you need to mix 15 mg:
- tar;
- sea buckthorn oils;
- salicylic alcohol.
After obtaining a homogeneous consistency, apply the ointment to the affected areas. It is also necessary to wrap areas with psoriatic rash with a plastic bag. After 1.5 hours, rinse the area where the ointment was applied.
Celandine oil
Boil a solution based on 5 tbsp over low heat for about 10 minutes. l. celandine and a glass of sunflower oil. Leave the resulting mixture in a dark place for 5 days. After receiving the oil, apply it to the inflamed areas.
Drug treatment
The main treatment consists of the following medications:
- Anti-inflammatory - non-steroidal drugs Diclofenac and Nimesulide. Reduce inflammation, relieve swelling and redness. The average course of treatment is 7-10 days.
- Sorbents – Smecta, Polysorb, Enterosgel. Remove toxins, reduce the period of exacerbation, improve liver function, which often suffers with psoriasis;
- Sedatives – Novopassit, Phytosed, tincture of valerian or motherwort. Eliminates excessive anxiety, reduces nervous tension.
- Antihistamines - Fenistil, Zyrtec, Suprastin, Fenkarol. Reduce itching caused by exfoliation and inflammation of the skin, remove the body's sensitivity to potential allergens.
- Glucocorticosteroid – Prednisolone intravenously. Quickly removes skin lesions, eliminates itching, and restores its structure.
- Antibiotic – Levofloxacin. It is used in case of bacterial infection in places where the skin is cracked.
- Enzyme preparations – Festal, Mezim, Panzinorm. They help restore digestion, problems in which are sometimes the cause of psoriasis.
- Immunosuppressant – Cyclosporine. Prevents the spread of disease foci by suppressing the proliferation of affected cells.
Hormonal and non-hormonal ointments are used:
- Salicylic acid – reduces inflammation, accelerates the resorption of plaques.
- Psorcutan – contains vitamin D, promotes the disappearance of lesions, increases the period of remission.
- Prednisolone ointment - quickly removes plaques and regenerates tissue.
- Alfozil, Colloidin - contain birch tar, have a wound-healing and disinfectant effect.
- Naphthalan ointment, Losterin - contains naphthalene. They have an anti-inflammatory, analgesic, vasodilating effect, eliminate peeling, and soften the skin.
Important! After the manifestations of psoriasis have been overcome, the skin must continue to be nourished and softened with creams, but the product must be of high quality and hypoallergenic.
Prevention
Exacerbation of psoriasis is easier to stop than to cure. To do this, you need to adhere to preventive methods:
- Follow a dietary diet. Alcohol is completely excluded from the diet, and smoking tobacco is also prohibited.
- When psoriasis occurs in winter, it is necessary to expose the skin to year-round ultraviolet irradiation. For this, you can sign up for a solarium or undergo physiotherapy. During summer progression, direct sunlight should be avoided.
- The use of medications should be carried out exclusively under the supervision of a dermatologist.
- Avoid emotional stress. Since it is stress that can become a provoking factor for exacerbation of psoriasis.
- Wearing comfortable clothes made from natural materials. In this case, it is necessary to limit friction, which can also cause an exacerbation of skin pathology.
- Strengthening the immune system. Optimal physical activity will not only have a positive effect on the body’s immunological response, but it can also improve your mood in life.
- Skin care. If moisturizing is necessary, it is better to use emollients purchased from certified pharmacies.
Psoriasis exacerbation, which is characterized by obvious symptomatic discomfort, can be stopped. If you follow all the dermatologist's prescriptions, adhere to dietary nutrition and drug therapy. In the presence of such a skin pathology, it is necessary in every possible way to support the immune forces of the whole body, which will help achieve long-term remission.
How to treat aggravated psoriatic arthritis
The treatment process for the disease is lengthy and requires strict adherence to the doctor’s recommendations. Today, experts offer five methods in the fight against psoriatic arthritis: drug therapy, local treatment, physiotherapy, physical therapy, and surgery.
Drug therapy
The technique involves taking tablets and injections.
- Anti-inflammatory drugs are prescribed to reduce inflammation - Diclofenac, Nimesulide, Meloxicam.
- Cytostatic drugs slow down pathological processes and are usually taken for two years. Among them, the most often prescribed are: “Methotrexate”, “Sulfasalazine”.
- Sedatives - “Persen” and “Afobazol” help with neurotic disorders and severe stress.
- Immunomodulators restore the body's protective functions. “Immunal” and “Licopid” are suitable for the complex treatment of arthritis.
- Immunosuppressants - Adalimumab and Etanercept suppress inflammation in psoriasis and arthritis.
- Multivitamin preparations - "Alphabet" and "Vitrum" are taken to strengthen the immune system and as a prevention of hypovitaminosis.
Local treatment
The method involves applying special gels and ointments to the diseased areas. Hormonal drugs such as Fluorocort and Sinalar have a greater effect . As an alternative, doctors offer salicylic ointment, as it soothes, accelerates the restoration of skin tissue and relieves inflammation.
Physiotherapy
Therapy is usually carried out during the period of weakening of the disease. The process uses therapeutic baths, mineral waters, paraffin baths and ultrasound. At this time, a joint massage is desirable.
Exercise therapy
The method is aimed at improving the motor functions of joints using a set of exercises for the feet and hands.
Surgery
When conservative therapy does not produce results or in fairly advanced cases, surgery is prescribed. Surgery is necessary when psoriatic arthritis affects large joints - the knee and hip. In this case, they are replaced with implants.
Scaly lichen is a serious chronic disease. Periods of remission alternate with exacerbations with enviable consistency. To avoid complications during relapse, you need to start therapy in a timely manner under the supervision of a doctor. Only comprehensive treatment prescribed by a doctor will help stop the progression of the disease.
Damage to nails and joints
Nails are appendages of the skin, so they are also involved in the psoriatic process. Nails change color and lose shine, become covered with stripes and grooves, small depressions in the plates make the nail look like a thimble. In the growth zone next to the periungual ridge, small red-yellow spots appear, and the free edge of the nail plate thickens and peels off, against which a fungal infection easily occurs.
Psoriatic arthritis is in most cases associated with skin lesions, but skin and joint changes occur independently of each other. In seven out of ten patients with arthritis, skin plaques appear before joint damage, in two - simultaneously, and in only one, arthritis precedes skin manifestations. This is a serious chronic inflammatory disease of an autoimmune nature.
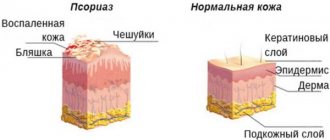
Psoriasis is definitely not an infection, so it is impossible to become infected with psoriasis. There is no single coherent theory of the causes of psoriasis, just as there is no single cause leading to the disease. The most scientifically confirmed theory is the immune theory of the development of the disease, when the immune system goes astray and an attack occurs against one’s own skin.
Failure in the immune system
The autoimmune theory is confirmed by the presence of huge accumulations of T-lymphocytes around each psoriatic plaque, as well as the sensitivity of the manifestations of the disease to immune drugs.
Recent viral or streptococcal infections (angina, scarlet fever), stress and poisoning predispose to autoimmune warfare. But for psoriasis to occur, a person must have genetic predispositions, and indeed such mutations have already been found in DNA; they precisely regulate the abnormal maturation of T-lymphocytes. The mutation will not necessarily lead to psoriasis, but without it there will definitely not be psoriasis. The likelihood of the disease increases by half if one of the parents is sick, but the mutation can not only be inherited, it can arise on its own - spontaneously.