What it is
Acne is a polymorphic, recurrent disease of the sebaceous glands. Acne is the most common skin dermatosis in young people, occurring in 95% of adolescents under 18 years of age and in 80-85% of young people from 18 to 25 years of age.
According to Ch. Colleir et al., during adolescence, the incidence rate is the same in women and men. “Late acne” is 1.5 times more common in women.
There are acne with signs of inflammation (papules, cysts, pustules) and without symptoms of bacterial spread (comedones). Papulopustular form is the most common clinical manifestation of acne dermatosis (70-80%).
Diagnosis of papulopustular acne
Only a dermatologist determines the type of acne by making a differential comparison with other types of acne. Also, this type of rash has common symptoms with inflammation of streptococcal and staphylococcal etiology. In addition, hyperpigmentation after the inflammatory process remains not only after a purulent rash, but is also a sign of dermatitis. Post-acne scars must be distinguished from vitiligo.
When diagnosing, the stage of development of the disease is determined:
- mild form, having comedones and up to a dozen papulopustular acne;
- medium - up to 40 eels;
- the severe stage is characterized by a large number of rashes. The disease is complicated by phlegmonous, conglobate or indurative acne. Depending on the form of the disease, a therapeutic course is prescribed.
Causes of acne
Acne is a complex, polymorphic disease. Because of this, it is common to associate the causes of acne with lifestyle, sleep and eating patterns, stress, lunar cycles, etc. However, only the hormonal theory of acne formation has been proven.
It is known that human skin has hormone-sensitive receptors; they respond to endocrine disruptions. The leading role in the pathogenesis of acne is played by hyperandrogenism - excessive synthesis of male sex hormones or increased sensitivity of dermal receptors to them.
Associated symptoms of hyperandrogenism in women:
- hair loss, oily seborrhea;
- Excessive male pattern hair growth on the body;
- increased sweating;
- polycystic ovary syndrome;
- irregular menstrual cycle, PMS, amenorrhea.
The German doctor S. Schmitz wrote that the skin is the largest endocrine gland in the human body.
The following facts support the hormonal theory of acne formation:
- acne occurs in 95% of adolescents during the period of endocrine changes;
- in the last phase of the cycle there is a short relapse of acne;
- in men, relapse is provoked by taking synthetic hormones, including steroids for muscle growth;
- acne often recurs during the climatic period in response to a decrease in estrogen levels.
The mechanism of formation of papulopustular acne
To a small extent, the severity of acne is influenced by diet, lifestyle, and skin care algorithm, but these factors do not provoke papulopustular acne.
No matter how unqualified cosmetologists and representatives of cosmetic brands try to speculate on this.
Mechanism of acne formation:
- Androgynous receptors in the dermis react to the production of androgens and stimulate the glands to synthesize sebum;
- Through the skin ducts, fat comes to the surface of the epidermis;
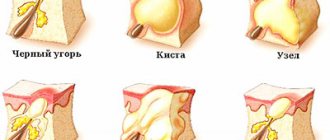
- Due to the increased density of the stratum corneum, sebum gets stuck in the pores, forming closed acne or comedones. When in contact with air, comedones oxidize and darken ("black spots" appear);
- The fatty environment in the sebaceous ducts creates more favorable conditions for the spread of anaerobic bacteria Propionibacterium acnes, streptococci and staphylococci. Microorganisms colonize the pores and provoke the appearance of inflamed acne (papules, pustules, cysts);
Characteristic signs
Papulopustular acne is a standard feature of acne. They occur in 80% of all patients. Among the “people” they traditionally have acne. What is this, from a medical point of view?
A papule is a hollow, superficial inflammatory nodule, up to 5 mm in diameter, without accumulation of pus. Papules look like mosquito bite marks (you can use the photo to guide you), they take a long time to go away and leave bluish or brownish spots.
A pustule is a papule plus a purulent peak filled with white or yellowish fluid. Heals after the bubble matures and bursts. May leave stains if not healed properly.
Pathogenesis
One of the pathogenetic mechanisms for seborrhea and acne is considered to be the activation of hydrolysis of sebum triglycerides by bacterial lipases, which leads to increased formation of free fatty acids and the development of an inflammatory process in the wall of the hair follicle.
It was found that with acne, not only the quantitative but also the qualitative composition of sebum changes, and these changes primarily relate to the concentration of linolenic acid. In the increased volume of sebum, the concentration of essential unsaturated linolenic acid decreases. Its deficiency may be due to both a lack of food and a deficiency of enzymatic systems that ensure its intake and distribution in the body. Linolenic acid is a major regulator of keratinocyte differentiation by inhibiting the expression of the enzyme transglutaminase (TG). This enzyme is involved in the synthesis of keratin 1st and 10th fractions, proteins - involucrin, loricrin and filaggrin - the main components; cementing intercellular substance of corneocytes. Increased TG activity causes retention hyperkeratosis in the infrainfundibulum of the pilosebaceous follicle (SVF). The predominance of the processes of proliferation and dyskeratosis over desquamation of the epithelium ultimately leads to the closure of the SVF duct and the formation of a comedon. A decrease in the concentration of linolenic acid also leads to an increase in the pH of sebum and a change in the permeability of the follicle epithelium. The barrier function is disrupted and conditions for the growth of microorganisms are created; on the surface of the skin and inside the follicles.
With acne, the processes of keratinization at the mouth of the hair follicles are also disrupted. The process of desquamation of epithelial scales from the canal of the hair follicle is regulated by a protein - profilaggrin, which is part of the spinous layer of the epithelium. In the cells of the granular layer, this protein is converted into filaggrin and is found in keratohyalin granules. The outcome of this aggregation is the transformation of the cell into a horny scale. With acne, there is an increased accumulation of both profilaggrin and filaggrin in the epithelium and, as a consequence, follicular hyperkeratosis occurs, which leads to expansion of the hair canal. Subsequently, the enlarged canal is filled with sebum and cellular detritus, which leads to its blockage and the formation of a comedon.
Obstruction of the SVF duct by comedones creates favorable anaerobic conditions for the proliferation of facultative anaerobes Propionibacterium acnes and Propionibacterium granulosum.
Long-term studies have shown that the inflammatory process in the sebaceous glands is caused by the following types of microorganisms: Propionibacterium acnes, staphylococci, mainly type II, and yeast-like fungi of the genus Malassezia. Antigens of microorganisms attract mononuclear phagocytes and neurophils to the SVF from the peripheral blood, which produce interleukins 1α, 1β and 8; tumor necrosis factor α, stimulate the complement system. These pro-inflammatory cytokines activate the enzyme cyclooxygenase, resulting in the formation of the main inflammatory mediator, leukotriene B4 (LTB4), from arachidonic acid. LTB4 activates neutrophils, T-lymphocytes, monocytes and eosinophils with their subsequent release of hydrolytic enzymes and nitrogen monoxide (NO). Destruction of the wall of the sebaceous gland with the release of its contents into the dermis causes the formation of an inflammatory reaction, which is manifested by papules, pustules, nodules and cysts.
Recent research evidence reconsiders the etiological role of Propionibacterium acnes. Thus, proinflammatory cytokines are considered to be the initiating factor of inflammation. In all comedones of acne patients, a high level of interleukin-1 is determined. Histological examination of fresh rashes showed that the perifollicular infiltrate is represented by mononuclear cells and T cells, and neutrophils appear later. Thus, today there are four main links in pathogenesis: hyperproduction of the sebaceous glands, follicular hyperkeratosis, microbial colonization and inflammation.
How to treat papulopustular acne
Only products approved by WHO and experts from the European Dermatological Forum will be considered.
The treatment protocol for papules and pustules includes methods aimed at:
- accelerating the regeneration of the epidermis, thinning the stratum corneum to prevent the occurrence of comedones (acids, retinoids, benzyl peroxide);
- removal of the inflammatory process (antibiotics);
Retinoids
Retinoids for acne are a class of drugs with an active form of vitamin A. For acne, only retinoic acid or tretinoin is used. Retinol Acetate or retinoic ointment give a very weak effect.
Tretinoin is the gold standard for acne treatment. It stimulates the renewal of epidermal cells, thins the stratum corneum and thickens the underlying dermal structures.
Retinoids are strictly contraindicated during pregnancy; they have side effects: dryness, peeling and increased sensitivity.
Preparations with tretinoin:
- Retin A;
- Renova;
- Acnelyse;
- Retino-A;
- Stieva-A;
- Airol;
- Locacid.
Retinol is also included in the popular cosmetic procedure “yellow peeling”.
Adapalene
In the CIS, medications containing tretinoin are not certified, so it is impossible to purchase the cream in a retail pharmacy chain. Domestic dermatologists prescribe ointments with adapalene. It is a vitamin A derivative with similar properties.
Preparations with Adapalene:
- "Differin";
- "Greyless";
- "Adaklin";
- "Klenzit."
Acids
All acids are used to treat papules and pustules. They provide antibacterial, regenerating and pigment-constricting effects.
Creams and ointments with azelaic acid (AA) have worked well. They are easier to tolerate compared to retinoids. AK dissolves comedones, exfoliates dead cells of the stratum corneum and acts on microorganisms as an antiseptic.
Preparations with azelaic acid:
- "Skinoren";
- "Azogel";
- "Azik-derm";
- "Skinoklir"
Peels with AHA and BHA acids also help in the treatment of acne: glycolic, salicylic, lactic, Jessner peel. They do not provide a preventive or prolonged effect, but provide quick results. To maintain success, cosmetologists prescribe home acid treatments.
Retinoids and acids thin the stratum corneum, accelerate the renewal of the epidermis and can provoke hyperpigmentation. Be sure to use creams with SPF and hide your face from direct sunlight.
Benzoyl peroxide
Benzoyl peroxide (BP) is a powerful oxidizing agent; upon contact with the skin, benzoic acid is synthesized, which exfoliates dead cells, frees follicles and provides a bacteriostatic effect.
Preparations with benzoyl peroxide:
- "Baziron";
- "Eclaran";
- "Ugresol."
Products with PB and acids gently disinfect and suppress the proliferation of pathogenic microorganisms. But the inflammatory process with papulopustular acne can be very intense, so sometimes it is necessary to use antibacterial agents.
Antibiotics
If there are more than 15 inflamed nodules with pus on the face, it is necessary to initiate antibacterial therapy. Clindamycin, erythromycin, and syntomycin are active against Propionibacterium acnes. In case of a large-scale inflammatory process (including on the back, chest), complex treatment with systemic antibiotics (tablets) is included.
Topical antibiotics help only in the treatment of papules and pustules. They are ineffective for subcutaneous cysts and comedones. It is advisable to use antibiotics together with keratolytics.
There are combination drugs on the market:
- "Duak" (clindamycin + PB);
- "Klenzit S" (clindamycin + adapalene);
- "Zinerit" (erythromycin + zinc).
A serious problem in antibiotic therapy is bacterial resistance to specific substances. Therefore, self-medication is contraindicated. Anaerobic microorganisms more often develop resistance to erythromycin, less often to clindamycin.
Is it possible to eliminate the cause?
90% of acne treatment is external therapy. A properly selected product helps normalize the skin, cure acne and post-acne. Treatment of hyperandrogenism is complicated by the fact that the specific causes of this metabolic disorder are unknown (only a genetic predisposition factor has been proven).
Combined oral contraceptives (COCs) with an antiandrogenic effect (Diane-35, Jess, Zhanin, Yarina) help to artificially correct the level of androgens. But COCs have a strong withdrawal syndrome and, in fact, also act superficially and temporarily. The effect on the skin after starting COC therapy occurs within 3-8 months.
Also, to correct the level of sex hormones, spironaloctone, metformin, and herbal dietary supplements with extracts of Saw Palmetto, Cohosh, and Evening Primrose are used.
Conclusion
Papulopustular acne is a complex, polymorphic and widespread disease. Characteristic symptoms of this form: the presence of inflamed acne with purulent elements (papules) and without (pustules). Modern treatment methods help get rid of rashes in 2-5 months.
The first choice medications are tretinoin and adpalene. Benzoyl peroxide and azelaic acid act more delicately and have fewer side effects; antibiotics are necessary to relieve severe inflammation.
But for successful treatment it is necessary to discard all pseudo-scientific therapeutic tools. Acne cannot be treated with tar soap, oatmeal, soda, calendula, or hydrogen peroxide lotions.
Treatment recommendations
The problem of acne treatment is far from resolved. The complex pathogenetic mechanisms of the development of the disease, as well as the existence of various clinical forms, determine the variety of treatment methods used. An individual approach to the selection of both systemic (for more severe or complicated forms of acne) and topical medications helps achieve good therapeutic results in patients with acne; the use of complex therapy allows one to achieve better results in a shorter period of time and achieve longer-term remission. Prescribing special auxiliary products for skin care makes it possible, during external or systemic treatment, to reduce the dose and frequency of use of drugs, to ensure a more comfortable condition of the patient’s skin. Acne therapy must necessarily be carried out taking into account the characteristics of the development and course of the disease, therefore, the success of treating patients with acne is possible only with close cooperation between the dermatologist, the patient and doctors of other specialties (endocrinologist, gynecologist, gastroenterologist and psychiatrist), as well as by prescribing drugs that would act on all the main links in the pathogenesis of the disease and were aimed at eliminating etiological and trigger factors.