Causes of acne
Acne on the feet occurs for a number of reasons:
- Fungus. You can catch the infection in crowded places (baths, saunas, swimming pools, water parks, beaches) if you neglect hygiene rules and do not use protective equipment. Mycosis manifests itself as slight redness on the sole, then peeling and irritation begin. Small pimples appear in the area between the toes and on the feet, which burst and merge into one large, weeping wound. The fungus affects the nail plates, changing the structure and color.
- Scabies. A contagious disease transmitted through handshakes and shared objects. Scabies appears as red blisters between the fingers and toes, and white stripes are visible under the skin - the burrows of the scabies mite. The disease is accompanied by severe itching at night, the harmful microorganism is activated and begins to spread throughout the body, including the palms, feet, and groin area.
- A pimple on your toe can appear as a result of poor hygiene. Miliaria provokes the formation of blisters on the skin of the heels, they burst, hurt, forming a favorable habitat for pathogenic bacteria.
- Infectious diseases. The clinical picture of many diseases begins with the appearance of a rash. It signals a progressive infection in the body. Chickenpox, measles, scarlet fever begin with small rashes on the skin, which vary in appearance. Then the temperature rises and other symptoms appear. These diseases are contagious and are considered dangerous, especially for a child, if treatment is not started in time.
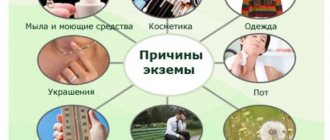
- Allergic reaction. Pimples on the feet may indicate the onset of an allergy. Cosmetics, household chemicals, and allergenic products can cause dermatitis of various etiologies, including between the toes and on the heels. A reaction to an allergen may not appear immediately, but after some time as a result of accumulation in the body. The component that provokes the rash can be determined in the laboratory. Allergies are characterized by itching and burning.
- Lichen. There are several types, each of which is characterized by the occurrence of acne. Pityriasis rosea is manifested by redness of the skin, on which blisters with watery liquid appear, framed by a red border. They begin to itch and become painful when pressed. The blisters are located at a certain distance from each other and do not merge into one large formation. Rashes with lichen planus look like bright red swellings that leave a mark even after complete recovery.
- Psoriasis. It is considered one of the types of lichen. It is impossible to completely get rid of the disease, but the accompanying symptoms can be eliminated. Psoriasis affects certain places - the elbow, knees, foot. First, small pimples appear, the skin becomes dry and begins to peel. Pimples increase in volume and form a larger affected area. Unlike lichen, psoriasis consists of a stage of exacerbation and remission. You should not delay treatment so that the disease does not spread throughout the body.
- Eczema, like psoriasis, cannot be completely cured. The disease affects the arms and legs. The skin becomes red, inflamed, and small blisters appear. There are two types of eczema: dry and weeping. When dry, there is severe peeling and itching. Then comes the weeping form, the most painful, the blisters burst, forming an open wound. As a result, there is a danger of additional infection. Eczema and psoriasis are considered autoimmune diseases that are aggravated by nervous stress and an unhealthy lifestyle.
- Insect bites. During a bite, blood-sucking parasites inject poisonous saliva, which leaves a mark in the form of a pimple. It may be very itchy, but you should not scratch it, as there is a risk of infection.
- Metabolic problems. A pimple on the heel may indicate gastrointestinal diseases. Impaired metabolism, poor nutrition, and lack of vitamins affect the skin, causing various dermatitis throughout the body.
Why do pimples appear?
The main factors that cause acne between the toes are:
- Scabies mite. Infection with scabies occurs as a result of bodily contact with a sick person or his clothing that has not been sanitized. Red, watery blisters appear on the toes and hands. In advanced cases, the infection spreads to other parts of the body. Pimples itch very much at night, when the mite is active.
- Allergic reaction. It is found on the legs of children and adults. Occurs as a result of an immune response to an allergen - preservatives in food, clothing made from unnatural materials, medications, foot cosmetics. A red or watery blister forms on the affected skin, accompanied by severe itching.
- Hyperhidrosis. If small pimples filled with clear fluid appear between your toes, this may be skin irritation due to excessive sweating. The condition is provoked by tight socks in the hot season and shoes with poor ventilation. Hyperhidrosis also occurs due to a hormonal disorder, vegetoneurosis.
- Uncomfortable shoes. Narrow and tight shoes cause compression of the toes, resulting in chafing - a small transparent blister that hurts a lot. Redness may form around the pimple.
- Psoriasis. It is characterized by the appearance of large raised pimples, severe itching and peeling. Most often it is formed due to stress or emotional shock.
- Fungi. Small white pimples appear. Accompanied by a floury type of peeling, the formation of cracks and wounds between the fingers, roughening of the skin, and brittle nails. You can catch the fungus in bathhouses, on the beach, or in a hostel. especially when using other people's personal hygiene items.
Measures to prevent diseases that cause rashes on the feet
- Some of the diseases described are autoimmune. This means that they are not contagious, and the cause of their occurrence lies within the body. Therefore, if such diseases were observed in parents, then it would be useful to be on the safe side. Learn to control your emotions, perhaps even enroll in thematic courses. Because the provocateur of such rashes is stressful situations, which are always impossible to avoid. But you can learn to respond to them without harming your health.
- Other types of diseases progress against the background of decreased immunity. Therefore, a course of vitamins in the off-season, proper nutrition, sports, healthy sleep, clean water, and the elimination of bad habits are the key to strong immunity. Even if it fails to resist the onslaught of bacteria, it will significantly ease the course of the disease.
- Elimination of allergens. An allergy is an individual reaction and can occur to any product or care product. But a number of foods, chemicals and cosmetics are known to be allergens. Avoid heavily colored and scented creams, deodorants, foot talcs and shower gels. Do not walk barefoot in places where there are aggressive chemicals. Refrain from “chemical” food and consumption of large amounts of products - classic allergens: citrus fruits, chocolate, red berries, honey.
- Treat bites, cuts, scratches—any damage to the integrity of the skin of the feet and toes—at home with antibacterial agents.
- If the disease has already taken you by surprise and the appearance of acne is accompanied by itching, trim your nails so as not to transfer the infection or fungus to healthy areas of the body.
- Give up bad habits. Provoking factors for triggering the mechanism of many autoimmune diseases are alcohol and smoking. Lack of sleep and nervous tension also aggravate the situation.
In public places (swimming pools, beaches, saunas, showers in a sports club), do not walk barefoot and do not use other people’s towels, brooms, or washcloths.
Such preventative measures will be an excellent basis for maintaining overall health. They will help prevent foot rashes and other dermatological diseases.
Prevention
After wearing a cast for a long time during a fracture, to prevent acne and cracks, you should pay attention to the care of the skin between the fingers, since the lack of air under the retainer contributes to the appearance of diaper rash and the activation of microbes.
To avoid pimples between your toes, you should choose the right shoes - from natural materials, strictly according to size and season. It is prohibited to use other people's slippers, socks, or tights. After visiting the beach and bathhouses, it is recommended to take a shower and treat your feet with an antifungal spray. You should also avoid shaking hands and hugging people you don’t know well.
What to do if a pimple appears?
If rashes appear on your toes and hands, you should consult a dermatologist. Depending on the etiology, the doctor prescribes the drugs shown in the table:
Medication groupName
| Against scabies | Sulfuric ointment |
| "Spregal" | |
| "Permethrin" | |
| "Crotamiton" | |
| "Benzyl benzoate" | |
| Antihistamine liniments | "Clarotalin" |
| "Lomilan" | |
| "Telfast" | |
| "Gismanal" | |
| "Zyrtec" | |
| Antifungal | "Lamikon" |
| "Nizoral" | |
| "Lamisil" | |
| "Ketoconazole" |
Causes of this disease on the legs
The skin of the feet is different from the dermis of the hands. The infections or causes of pimples in this area are sometimes the same, but often they are different. For example, one of the main sources of the formation of such acne is atopic dermatitis. The symptoms are watery pimples that you want to constantly scratch.
This allergic reaction is especially painful in children. They don’t understand and are constantly scratching at such formations. As a result, wounds open and microbes enter. This contributes to their even greater spread. For children, it is worth coming up with special means that can be put on their hands so that when trying to scratch such a pimple, the child cannot do this.
Red pimples between your toes may be the first sign of scabies. This is the ideal situation to take action. If you start using the necessary medications at least for a day, you can wait much longer for the result. Therefore, as soon as you see something similar in yourself, go either to the doctor or to the pharmacy. Do not exclude the option of communicating with the doctor by phone. Usually the patient tells the symptoms and the doctor can immediately make a diagnosis. Don't hope that everything will go away on its own. The scabies mite never goes away on its own; it is necessary to influence it in order to stop the process of its spread. If you start it, then after a short time it will no longer be possible to avoid treatment with antibiotics.
Features of the formation of piezogenic papules on the heels
-Dermatology-Rash
Piezogenic heel papules are a diagnosis often diagnosed in athletes involved in athletics and weightlifting. Formations on the foot appear after active exercise; at rest they do not cause discomfort, do not cause pain, or create a cosmetic defect.
What are piezogenic papules and what do they look like?
Formations on the heel appear against the background of constant stress. Adipose tissue is enclosed between fibrous fibers that form the septa. It acts as a shock absorber on the foot. When there is excess pressure on the leg or the integrity of the capsules is damaged, lipid tissue leaks into the subcutaneous tissue.
Piezogenic heel papules are bulging fatty tissue of the foot. The diameter of the attributes is from 0.8 to 1.2 cm, the elements correspond to the color of the skin, and may have a yellowish tint. They are soft, not fused to the epidermis, and disappear when pressed.
Histological examination of the papule reveals lipid tissue. Doctors diagnose the absence of degenerative changes in the ligaments and muscles of the foot.
Piezogenic disorders in the heel area are more often detected in overweight patients and individuals who, due to their occupation, have to be on their feet for a long time. A large category of people suffering from the disease are professional athletes.
The disease affects women, and sometimes papules appear in children.
Causes and factors of occurrence
The main reason for the formation of piezogenic formations on the heels is pressure on the limbs, weakness of the connective tissue. Factors contributing to the development of the pathological process:
- heredity;
- disturbances in the development of fibrous capsules, their weakness, low elasticity lead to the appearance of papules;
- A history of rheumatism contributes to the occurrence of a piezogenic rash;
- inflammatory processes in the foot, heels;
- deficiency of nutrients, vitamins;
- heart defects as a complication of rheumatism;
- excess body weight – papules develop in patients who are over normal weight;
- long-term static tension in the legs - people who are professionally involved in sports, hairdressers, and salespeople suffer from piezogenic formations.
Symptoms of the disease
Formations are found on the lateral, dorsal, and medial surfaces of the heels. Fatty swellings on the legs and palms are rarely diagnosed.
Piezogenic foot papules cause symptoms:
- soft neoplasms that do not cause discomfort;
- shape – spherical;
- color – white, shades of beige, yellow;
- with small sizes they do not provoke heel pain or discomfort when walking. Unnoticeable at rest;
- with a significant diameter of piezogenic units, patients complain of unpleasant sensations from papules while moving or while standing. The nature of the pain syndrome is oppressive and exhausting.
Unpleasant symptoms develop due to compression of adjacent tissues.
Features of the treatment of papules on the heels
The WHO documents do not indicate the specialization of the doctor involved in the elimination of piezogenic formations. If symptoms occur, contact an orthopedist, dermatologist, or oncologist to diagnose the risk of neoplasms for malignant nature, bone injuries, and ligaments of the foot. Pathology is distinguished as social; it has recently begun to be described in the medical literature.
Treatment of piezogenic heel papules is carried out in cases of significant size of the heels, discomfort, and pain when moving. Drug therapy, surgical interventions, physiotherapy, and acupuncture are used.
Conservative
At the initial stage, the patient is examined and the heel is examined. The doctor excludes the possibility of developing fibroids, wen, rheumatism, and helminthic infestations. Piezogenic samples are not taken for histological examination: the papule does not degenerate into carcinoma.
Traditional medicine offers treatment methods:
- a solution of betamethasone and bupivacaine - a combination of glucocorticosteroid and anesthetic is injected into the affected area on the heels. This method is not included in the therapeutic technologies for managing patients with fatty protrusions on the foot; it promotes the resorption of piezogenic neoplasms.
- destruction of elements is a minimally invasive method of treating papules;
- the use of drugs from the NSAID group - with the development of pain, inflammation in the feet due to tissue compression;
- the use of underwear, caps that compensate for the load on the limbs;
- injection of corticosteroids into the lesion: they promote the resorption of piezogenic elements on the heels;
- physiotherapy and acupuncture reduce the number of papules on the body;
- reducing the load on the foot.
Additionally, normalization of the diet, lifestyle changes, and drinking enough water are indicated.
Surgical
Surgical treatment is prescribed for significant papules, the presence of pain caused by piezogenic bulging, and signs of compression of healthy tissues.
Surgical methods for treating formations in the heel area:
- Removal using electric current is a minimally invasive procedure that does not require preparation or hospitalization. Local anesthetics are used during the procedure. The likelihood of bleeding or infection with pathogenic flora during electrical destruction of piezogenic bulges on the heel is minimal.
- Husking of adipose tissue is indicated for voluminous neoplasms. Manipulation to get rid of papules is carried out in a hospital setting. The method of pain relief is discussed with the patient, selected individually, and local anesthesia is often used. After removal, the doctor will explain the rules for caring for the wound.
When manipulating piezogenic growths on the heel, there is a risk of bleeding and secondary infection; after the procedure to remove the papule, sutures are applied.
During the rehabilitation period, it is mandatory to wear caps, underwear, and avoid putting any weight on the affected leg. After healing, it is recommended to change your occupation to prevent re-infection.
Traditional methods
There are methods to alleviate the condition and eliminate discomfort from touching the heel. Traditional medicine does not have recipes for the treatment of piezogenic swellings. Home methods are combined with traditional therapy.
Do you need advice from an experienced doctor? Get a doctor's consultation online. Ask your question right now.
Ask a free question
Histological examination of the papules will reveal adipose tissue without signs of degeneration or pathological changes. You can try home methods for treating wen, stimulating the spontaneous opening of the lipoma on the heel, the expiration of the contents of the piezogenic capsules. These are various lotions, ointments, tinctures of medicinal herbs.
The procedures are hazardous to health, there is a risk of secondary infection with papules, the development of a diffuse inflammatory process, phlegmon or abscess, gangrene, and sepsis. You should not attempt to independently eliminate piezogenic nodules on the heel; untested methods are contraindicated for treating children, adolescents, and pregnant women.
Possible complications and prognosis of the disease
Exacerbations due to the advanced state of piezogenic bulges on the heels are associated with compression of surrounding tissues. Dangerous outcomes:
- pain when moving, at rest in the area of the papule;
- subcutaneous hemorrhages;
- inflammatory processes;
- phlegmon, abscess formation;
- spontaneous opening of the piezogenic capsule with the formation of a large wound on the heel;
- surface infection;
- gangrene, sepsis.
The prognosis of the disease depends on the size of the papules, their number, and the patient’s response to treatment. Therapy is being developed, medications are being selected: there is no universal method for eliminating the disease.
If you resort to self-diagnosis and use unverified recipes for the treatment of piezogenic nodules on the heels from folk sources, you can expect unforeseen consequences, an advanced stage of papules, and an exacerbation. If growths appear on the foot, you need to consult a doctor and undergo a comprehensive examination.
The article has been reviewed by the site editors Link to the main publication
Didn't find suitable advice?
doctor or see all questions...
articles:
Loading…
Source: //VashaDerma.ru/dermatologiya/syp/pezogennye-papuly-pyatok
What causes rashes on feet
Acne and other pimples on the face rarely signal problems that require immediate solutions. Typically, such rashes are provoked by factors accumulated in the body: intoxication, hormonal imbalances, and so on. Changes in the quality of the dermis of the feet and toes most often manifest themselves sharply and in an acute form. And the problems that these phenomena indicate may require urgent medical intervention. Among the provoking factors are:
- infectious diseases;
- allergic reactions, dermatitis;
- psoriasis, eczema;
- cancer;
- other.
Even a person with a medical education cannot always make the correct diagnosis based on the type of rash alone. In most cases, additional laboratory tests are required.
Allergy
The most common and most harmless cause of rash on the feet in men and women is an allergic reaction. It manifests itself as an irritating factor that affects the body both from the inside and outside. When trying to figure out what caused the reaction, don't throw away products you've used before. Indeed, for allergies, the cumulative effect also becomes important, when something that previously did not cause dermatological problems can today manifest itself as a rash. There is no point in diagnosing allergies on your own. It has many faces and can masquerade as other diseases, so it is important not to confuse it with something more serious. With allergic reactions, flaky scales, red spots, blisters and papules may appear on the feet. There may be many or one or two. Itching is also not obligatory, but a possible phenomenon.
Infectious diseases
Some viral diseases manifest themselves as rashes and “pimples” on the skin of the feet and other parts of the body in the early stages. Measles, chickenpox, scarlet fever are an incomplete list of infections that are characterized by rashes on the body. And none of them can be called harmless. Therefore, it is important to diagnose the disease in a timely manner and begin treatment. Such diseases are extremely contagious and it is unacceptable to decide how to get rid of their manifestations on the advice of grandmothers and friends. Rashes with such ailments look like red blisters or papules and may itch. Most infectious diseases are characterized by an increase in temperature, a change in the color of mucous membranes, and a deterioration in general health. Therefore, rashes are not the only symptom, but one of the first to appear. It is important not to miss the moment, pay attention to it and seek help from a doctor.
Psoriasis
Eczema
The causes of this disease have not been clarified to this day, so it is not yet possible to cure it completely. It can be provoked by: dysbacteriosis, deficiency or excess of vitamins, malfunctions of the digestive organs, kidneys, weakened immunity and other factors. Eczema spreads, most often, on the extremities, manifesting itself first as itchy redness, and then as blisters on the affected areas. The disease has several stages and types, and each subsequent one is controlled worse and worse. Therefore, timely medical intervention is necessary. The disease most often occurs in a dry form, but sometimes a weeping form occurs, causing even greater discomfort on the feet due to watery rashes.
Some types of lichen
Psoriasis is also a representative of lichen, but there are other types of this disease that are completely different from it. These include:
- Shingles. It is characterized by an increase in temperature with significant lesions, rashes in the form of many watery blisters with cloudy contents, pain and itching in the initial stages;
- Pityriasis rosea. During this disease, spots appear on the skin and rashes in the form of blisters with a red border. Sometimes they are accompanied by slight pain, but they never merge with each other, which is typical only for this type of lichen;
- Lichen planus is a non-contagious disease. Rashes in the form of bright papules are very characteristic and do not cause difficulties for the doctor in diagnosis. After recovery, red spots remain at the site of the rash for a long time.
Each type of lichen has its own treatment, therefore, even if you suspect you have one or another type of disease, consultation with a doctor to prescribe the correct therapy is mandatory.
It is important to understand that lichen itself, and other dermatological reactions with which it can be confused, can be signals of other, more serious diseases, including various types of cancer.
Mycosis
This name summarizes several types of foot and toe diseases caused by fungi. The insidiousness of this illness is that it appears and disappears for no apparent reason, creating the illusion of recovery. The disease begins with peeling, often in the area between the fingers. Without treatment, it progresses to more severe forms, characterized by a blistering rash in the arch of the foot. Affects nails, changing their shape, structure and sometimes leading to their loss.
Scabies
A contagious disease transmitted by contact with the skin of a sick person. The disease is characterized by a red rash localized between the fingers, on the feet, in the genital area, on the wrists and other parts of the body. It is caused by the scabies mite, which moves under the skin, leaving passages in it. In the evening, microorganisms become more active, causing itching, which is difficult to ignore. Scratching “pimples” leads to secondary infection (for example, staphylococcus). In this case, the “pimples” become purulent and watery.
Whatever disease you diagnose yourself with, based on descriptions and photographs on the Internet, do not neglect going to the doctor. Especially if, in addition to rashes on the feet, other changes in the condition of the body are observed.
White balls on the heels - piezogenic heel papules - answers and tips for
If a lump appears on the foot that causes pain, it should be classified in order to prescribe adequate therapy. The characteristic shape of the seal resembles a ball, the dimensions of which range from 1-2 mm to 3-4 cm. When you press on the seal, a sharp pain occurs.
Corns
With keratinization of the skin on the feet, which is caused by improperly selected shoes, obesity, excessive sweating, flat feet, arthritis, etc. This reason is the most common.
Corns can be flat, dry, raised, with or without rods. They have a yellowish-brown tint, a rough skin surface with reduced sensitivity to external influences.
In some cases, cracking of the foot is possible, accompanied by pain during increased physical activity. In the absence of timely treatment, the foot may become deformed, displaced, and the ball of the big toe may become enlarged.
Corn
A distinctive feature of calluses is their shape, which is a round, limited area of skin on the heel or toes, which is accompanied by pain even with slight pressure. Often, calluses can appear in a child, which is associated with the wrong choice of shoes, flat feet and injuries.
Calluses can be wet or dry. Wet calluses are the most dangerous, since they contain an accumulation of fluid (blood, serous exudate), which can leak out when the callus is traumatically damaged. As a result, there is a possibility of infection of the wound surface. In addition, wet calluses can transform into dry calluses, but with deeper roots.
It will take a lot of time to completely get rid of calluses. If the inflammatory process develops, antibiotic therapy may be prescribed, and if the symptoms are severe, surgical intervention is recommended.
Warts
In appearance, warts are very similar to calluses. The color of the resulting bumps practically does not differ from the color of the skin, and the foot is rough on palpation. When pressing on the plantar wart, acute pain is observed. The difference between a wart and calluses is the presence of a dark dot in the middle, but if the wart grows deeply, it is quite difficult to notice it.
Warts are of a viral nature and are classified in medicine as benign neoplasms.
The strains of the virus responsible for the formation of warts on the sole of the foot are not dangerous. The virus is not capable of transmitting from person to person and is activated only in a humid, warm environment. For a wart to appear, a starting point (an abrasion, injury, etc.) is required, as well as a weakening of the body’s immune defense.
Atheroma
A seal of this type is quite movable and soft to the touch. The cause of atheroma formation is the inflammatory process in the sebaceous gland. During physical activity on the lower extremities, pain symptoms are likely to occur, as well as various types of deformities in the arch of the foot.
The main condition for the success of therapy for atheroma is careful adherence to hygiene measures, prevention of damage to the integrity of the skin, normalization of immune defense and the choice of the right shoes.
Thrombophlebitis
This disease is accompanied by compactions in the lower extremities and is characterized by a chronic course. In the process of disruption of blood flow, a clot (thrombus) is formed, diseased veins become inflamed, and a dark blue compaction appears at the site of development of the pathological process. Even with slight pressure on the tubercle, sharp and severe pain occurs.
This is what thrombophlebitis of the deep veins of the limb looks like
Bursitis
This disease in most cases is characterized by a benign tumor-like formation filled with gel-like contents. On palpation, the seal is round, mobile, elastic and soft.
Painful symptoms occur as a result of physical stress on the affected leg. Therapeutic measures for bursitis include immobilization of the affected limb, wearing comfortable shoes, and physiotherapy.
In case of chronic development of bursitis, a surgical puncture of the bursa is performed, followed by washing the cavity with antibiotics and prescribing hormonal drugs.
Phlegmon
You can also read: What is a spur on the foot
Even small wounds or cracks in the foot can cause the formation of a seal with phlegmon. Often, phlegmon develops after boils, carbuncles and long-term non-healing ulcerative neoplasms. The site of inflammation is red and hot to the touch, there is acute unbearable pain, weakness and deterioration in the general condition of the patient.
Phlegmon requires mandatory treatment, including surgery, since various complications may lead to amputation of a limb, and in some cases the patient may die. Therefore, at the first symptoms of the disease, you should immediately contact a medical facility.
Heel spurs
With increased calcium deposition, heel spurs may form. In this case, the soft tissues of the foot compress the nerve endings, causing unbearable pain to the person. Typically, the incidence of heel spurs within the joint increases in older age, due to wear and tear of the fatty tissue on the bottom of the foot.
Treatment is carried out with external medications and intra-articular blockades, which effectively relieve the inflammatory process, relieving pain symptoms. In the absence of a positive result, surgical intervention is recommended.
Keratoderma
This disease is extremely rare and the causes of its occurrence are not fully understood. Presumably, genetic mutations can lead to keratoderma. This group includes several types of dermatoses accompanied by impaired keratinization. Externally, the growth resembles a yellow-brown tubercle, slightly rising above the skin with the presence of small depressions on it.
Keratoderma belongs to the group of dermatoses that are accompanied by a violation of the keratinization process
Seals cause discomfort to the patient, and in some cases they may indicate the development of a serious inflammatory process in the body. It is recommended to treat the disease as an internal autoimmune disorder. Characteristic symptoms of keratoderma are lack of pain and constant itching.
Multiple hernias of fatty tissue of the heels are also called piezogenic heel papules.
They are usually round, slightly protruding skin-colored lesions.
They do not have a large diameter and slightly reach 1 cm. They occur during a long standing position and with a heavy load on the legs, long running in people with heavy weight. It is more common in women. Painful sensations usually do not cause and usually disappear when the legs are horizontal.
Depending on how deep the nodules are located in the skin, the following types are distinguished:
- Superficial. Occurs in the epidermis or upper layers of the dermis. They almost always do not cause pain; the size ranges up to 5 mm. Color can vary from pale pink to deep red. This skin element passes without a trace (no scars are formed).
- Deep. Occupy almost all layers of the dermis. They hurt, the color can vary from red to bluish. Resolution of the nodes occurs with the formation of scars.
- Cysts. A type of deep papules that exist for a long time. If the contents of the nodule have not been completely eliminated, then it can fester again with the additional formation of a fibrous capsule.
Depending on the size and shape, nodules are divided into:
- Miliary papules (cone-shaped). They resemble a millet grain. Most often located around hair follicles.
- Lenticular papules (flat). They are slightly larger in size and shaped like lentils.
- Nummular - reach the size of a coin.
Below is a picture showing flat, single papules on the skin. The photo shows characteristic formations that resemble lentils in shape.
Neoplasms on the feet
One of the causes of pain and lumps on the feet and soles is calluses—clumps of keratinized, dead tissue on the soles of the feet. They differ from calluses in that they do not ooze.
When walking, during their appearance, a painful sensation occurs, which is accompanied by a burning sensation. Over time, if not properly cared for and treated, seals can appear with deep bloody cracks in the heels.
These painful formations are yellow and grayish-yellow in color. As a rule, their appearance is provoked by the following factors:
- tight, uncomfortable shoes;
- heavy weight;
- diseases of internal organs;
- flat feet.
In medical practice, two types of corns are distinguished. Dry and with a core that grows deep into the skin, it is very difficult to remove. Because of this feature, they were given the name thorns, which cause pain when pressed on them.
You can get rid of such a formation on your foot by changing your shoes to looser ones and visiting a cosmetology office. There, with the help of special procedures, all formations on the foot will disappear in several sessions.
As a rule, their advanced forms are treated with cryodestruction, the essence of which is the use of nitrogen.
Despite the fact that the procedure is painful and has a high cost, it is in demand among salon clients because it leaves no scars and there is no chance of relapse.
Often, a laser is used to remove corns, which painlessly removes dead cells of the formations and does not affect healthy skin. With this method of treatment there is no chance of wound infection. Ointments and gels that have a softening, antiseptic and analgesic effect also help treat corns:
- Keratolytic agents - Lekar cream, Superantimozolin, Bensalitin ointment, cream paste for 5 days.
- Special plasters against corns - Salipod, Chinese plasters ShuyangSuan.
- Pencil for getting rid of corns - Wartner, Compeed.
- Women's medicinal socks with herbal infusions, with a relaxing effect.
- At home, you can use baths and compresses with the addition of essential oils.
Preventing a bump on the heel
Have any unpleasant protrusions started to appear after a run? In a calm state, they are practically invisible, they do not hurt, but they spoil the aesthetic appearance of the feet.
Besides, what if it’s a tumor? The doctor surprised me with the diagnosis of “piezogenic papules.”
Source: //ocrb.ru/problemy/v-pyatke-kak-budto-sharik.html
Treatment methods
The method of treatment depends on the cause of the disease. A dermatologist is a doctor who deals with skin diseases and will be able to make an accurate diagnosis and prescribe complex therapy:
- for mycosis, antimycotic drugs (Lamisil, Exoderil) are prescribed, the action of which is aimed at destroying the fungus;
- scabies can be treated at home using ointments: benzyl benzoate or sulfuric (during treatment it is worth isolating the patient to prevent infecting others);
- infectious diseases should be treated under the supervision of a doctor who prescribes appropriate therapy;
- in case of an allergic reaction, you need to identify the allergen and exclude it from the diet or environment (be sure to take antihistamines);
- rashes from lichen, psoriasis, eczema are treated with antibacterial ointments and corticosteroids (in severe cases, a course of antibiotics, sedatives);
- diseases of the gastrointestinal tract are treated inpatiently while following a diet (pimples as a symptom go away very quickly with complex therapy);
- insect bites are lubricated with panthenol-based preparations (Bepanten, D-Panthenol).
Pimple between toes how to treat?
Poll: When did your acne appear? (Number of votes: 1743) I’ve been suffering all my life For a couple of years About a few months More recently To vote, click on the desired answer option. Results
Small bubbles with a small amount of liquid inside can be left at your discretion and without treatment, as they can quickly go away on their own.
You should never resort to piercing the blister, which can cause bleeding and other problems associated with the infection and spread of the pimple. Puncture of the blister will put you at risk of infection from bacteria in your bloodstream.
You can separate your toes and help relieve pressure on the little blisters by using medical-grade gel pads, which can be purchased at the drug store. Keep the webbed space between your toes clean by washing it regularly with soap and water, wiping it with a clean cloth. Soak your feet twice a day. a day in a mixture of white vinegar and epsom salts is also very beneficial.
In the case of large blisters, careful piercing is still recommended, because if they are left to grow, they will be painful and may burst on their own. To pierce a pimple between the toes, first make sure that your hands are clean and sterilize them along with the piercing needle with alcohol.
Older methods include sterilizing the needle with fire, but doctors strongly advise against this method of piercing because carbon particles can get into your skin and aggravate the wound.
You can also prick watery pimples by using sterilized fingers to gently squeeze the liquid out from inside the pimple. Do not remove the skin around the popped pimple, as this is a protective barrier for the raw skin underneath.
Apply an antibiotic cream to kill bacteria and take care to wrap the punctured pimple with a tight bandage to keep it clean.
Keep an eye on your wound and look for strange fluid that may be white or yellow in color. Such fluid, red streaks and warm skin around the wound could be a sign of infection and that you have done something wrong. The astringent properties of aloe vera gel are great for soothe the wound and may help prevent infection.
Periodically remove the bandage and soak in epsom salt. Place a new bandage after soaking and keep the bandage until the skin begins to heal.
For blisters with fungal infection, keep your feet super clean and dry and use an antifungal cream.
Why do pimples itch and how to get rid of itching in 1 hour!
Possible complications
You should not ignore the problem or self-medicate; even ordinary acne can cause serious consequences. Acne that appears on the heels can trigger the onset of such a serious disease as heel fasciitis. With rashes on the extremities, there is a risk of infection, which can lead to gangrene, and in advanced cases, amputation. Terrible complications can be avoided if you seek medical help in a timely manner and follow preventive measures:
- monitor hand and foot hygiene, use antibacterial soap after visiting public places;
- carefully care for the skin of your feet using moisturizers;
- do not walk barefoot in the sauna or swimming pool;
- lead a healthy lifestyle, give up bad habits;
- eat a nutritious, varied diet, including vitamins and minerals in the diet;
- avoid stress and overexertion.
Skin defects cause aesthetic discomfort and unbearable pain, which changes the usual way of life. You should be attentive to any changes in the body in order to quickly get rid of a delicate problem. Timely medical care and medications will help restore health and beauty to the skin without relapses or negative consequences.
When is a visit to the doctor necessary?
Rashes on the feet are aggravated by the need to wear shoes. In winter, feet may sweat, increasing the itching; in summer, wearing open shoes increases the risk of infection. The picture can be blurry, and primary rashes can be mistaken for dropsy, abrasions, or insect bites. Therefore, remember that it is necessary to consult a doctor if you have the following symptoms:
- The rash is accompanied by fever;
- The reaction quickly spreads to other parts of the body;
- Similar signs were found in people with whom you were in direct contact;
- The resulting rashes are filled with purulent contents;
- The rash is located in a place where it is constantly injured when walking, leading to the spread of infection;
- Any rashes or acne in a child, regardless of location, must be examined by a doctor. If a rash on the foot appears in a family member with a child, then consulting a doctor is also necessary, since many diseases that manifest as rashes are extremely contagious.
Rashes on the feet, unlike acne, often indicate a progressive disease in its acute form. Therefore, self-medication is dangerous both for the sick person and for others. Treatment of such problems is permissible at home, with the permission of a doctor and strictly following his recommendations.
Piezogenic papules of the heels treatment
A piezogenic foot papule is a hernia of fatty tissue in the heels. This formation ranges in size from 8 to 10 mm in diameter and is the color of the skin. They develop with excess pressure on the feet as a bulging of adipose tissue into the subcutaneous tissue. In English, “piezo” means pressure. This factor is the main one in the formation of fatty hernias.
What are and reasons for the appearance of piezogenic papules
Have any unpleasant protrusions started to appear after a run? In a calm state, they are practically invisible, they do not hurt, but they spoil the aesthetic appearance of the feet.
Besides, what if it’s a tumor? The doctor surprised me with the diagnosis of “piezogenic papules.”
Normally, fatty elements in the tissue of the heels are located in peculiar capsules that form fibrous septa. Lipid tissue plays a shock-absorbing role, reducing stress on the feet.
With increased physical activity and disruption of the formation of fibrous fibers, adipose tissue can appear in the subcutaneous space. In this case, a piezogenic heel papule is formed on the leg.
Causes of the pathological process:
- genetic predisposition;
- history of rheumatic heart disease;
- increased static stress in the legs of athletes - figure skaters, speed skaters;
- excess weight in stages 3 and above of obesity.
Features of piezogenic papules on the heels and feet
The main group of patients with this pathology in the legs are representatives of the fair sex. The disease is rare in men, although cases of such neoplasms in children have been described in the medical literature.
During histological examination of the samples, doctors noted the absence or degenerative changes in the tissues of the fibrous septa of the feet.
The location of these neoplasms is on the lateral, dorsal and medial surfaces of the heels, although the medical literature describes cases of the development of piezogenic papules on the lower leg, arch of the foot and wrists.
- soft formations;
- color white, natural or yellowish;
- painless, but in some cases patients complained of discomfort when pressed after prolonged physical activity. Unpleasant sensations develop due to ischemic compression of the surrounding tissues by the neoplasm.
Traditional and non-traditional treatment
If any tumors appear in any location, you should consult a doctor. And although the WHO protocols do not indicate the specialization of the doctor who should deal with such formations, it is recommended to visit a dermatologist, oncologist and orthopedist.
- Features of papules with chickenpox
- Why can a wen become inflamed?
- Effective remedies for warts
The neoplasm should be differentiated from fibromas, leiomyomas, lipomas, rheumatic plaques, and helminthic infestations. Biopsy is not indicated. But if the study was carried out, then thinning or destruction of the fibrous septa and compaction of the tissue of the feet are detected.
Skin formations are a kind of lipoma, as they consist of adipose tissue. The likelihood of degeneration into a malignant neoplasm is minimal. Such cases have not been described in the medical literature.
Treatment of this pathology is carried out only if the papule causes discomfort or pain.
What does official medicine offer? There is no WHO protocol for the treatment of this disease, since the disease is social in nature and as a pathology was described in the medical literature relatively recently.
How to treat a tumor on the heels:
- injections of betamethasone and bupivacaine - this is not a standard of treatment, but the literature describes cases of getting rid of pathology after a course of these drugs;
- electrical destruction of neoplasms;
- physical therapy techniques such as electroacupuncture;
- a number of orthopedic measures;
- wearing heel caps and special underwear;
- injection of steroid drugs into the lesion;
- for pain, the use of NSAID painkillers is indicated;
- treatment involves rest, reduction of static and increased dynamic loads on the feet;
- If persistent pain develops, surgical desquamation of tumors is recommended.
What are the types of acne?
The main pimples that form between the toes of the lower extremities are shown in the table:
VarietyCharacteristics
| Pustule | White pimple filled with pus |
| Occurs when pathogenic bacteria enter a microwound on the skin | |
| Papule | The large red nodule contains an infiltrate - an accumulation of dead cells mixed with blood and lymph |
| Blister | Large pimple filled with clear fluid |
| After opening, a wound is formed | |
| Milium | White subcutaneous pimple, firm to the touch |
| Made from keratin |