A thermal burn is tissue damage that occurs under the influence of high temperatures. As a rule, the first symptoms of damage occur when the skin is exposed to a substance heated to 55 degrees Celsius or higher.
There are 4 degrees of tissue damage in total. The fourth is considered the most dangerous, since it damages not only the deep layers of the epidermis, but can also be accompanied by complications in the form of infectious inflammation or malfunctions of the respiratory and cardiovascular systems. Today we will try to understand the degrees of thermal burns and their treatment.
What is a thermal burn
Before studying information about the treatment of thermal burns, you should understand the very concept of such damage (Figure 1).
So, thermal is a burn that was received as a result of contact with a liquid, solid or gaseous heat source. These include regular open flames, steam and hot liquids.
Statistics show that more than 80% of all thermal burns were caused by contact with flame. Damage from hot liquids follows by a wide margin.
The stage of damage is determined by the number of injured layers: the more there are, the higher the degree. In addition, such damage is usually divided into complete, partial and superficial. The severity of the injury is indicated as a percentage relative to the total area of the skin.
Figure 1. Burns are a common household injury.
To roughly estimate the affected area, the so-called “rule of palm” is usually used. The area of skin on it corresponds to one percent of the total body area. Depending on the degree of the burn and its area, a general description of the patient’s condition is drawn up and treatment is prescribed.
ICD 10 code
The ICD 10 code is used to classify all diseases and injuries. This is an international statistical system that is used to classify all diseases, injuries and other health problems into different types.
Characteristics of thermal damage
In the International Classification of Diseases (ICD), a thermal burn is damage to the epithelium or deep tissues of the body from a heat source of high temperature (fire, steam, boiling water, hot objects).
The leading place among thermal injuries is occupied by burns from flames - 70%. Injuries due to scalding and contact with electric current account for 25%, under the influence of other factors - up to 5% of recorded cases.
This is interesting: First aid for a scorpion sting
A thermal burn damages various layers of the skin - from the superficial epidermis to the subcutaneous tissue, and in severe cases to the internal organs. Injuries are classified according to factors of depth and extent of pathology. Complex therapy and long-term recovery are associated with the destructive effect of the damaging factor on the protein involved in cellular renewal.
Characteristic signs
It should be immediately clarified that the symptoms of burns, although similar in stages, directly depend on the degree and area of damage (Figure 2).
Local signs include:
- Severe and sometimes unbearable burning and pain in the area exposed to the heat source.
- At the initial stage, redness appears, which is later supplemented by swelling and a local increase in temperature.
- Already at the second stage, small bubbles filled with a yellowish liquid begin to appear. At the third stage, they transform into burns with blisters, and the largest of them can merge into one.
- Also at the third stage, sensitivity in the affected area decreases, and a scab may begin to form at the site of the blister, with further suppuration of the wound.
Figure 2. The affected area turns red, swells and begins to hurt.
The fourth stage of the burn is considered the most terrible. Despite the fact that there is no pain with such an injury, the tissues become charred, which leads to burn disease. It affects not only the skin, but also other organs and systems. A person with such an injury requires emergency medical care, long-term treatment, and often surgery.
Let us consider in more detail the degrees of thermal burns and the causes of their occurrence. This information will help you avoid such injuries.
General recommendations
In the event of a thermal burn, first aid should be provided by others who witnessed the incident. First of all, it is necessary to move the victim to a safe place and save him from further exposure to thermal energy. Then you need to evacuate the patient to fresh air and clean the mouth and nose of possible combustion products. If the person is unconscious, the person should be placed on their side so that in case of vomiting the airway is not damaged.
The first first aid for thermal burns is to cool the wound with cold water; it is not recommended to use ice or compresses as a coolant.
You should also avoid applying folk remedies such as vegetable oil, sour cream or any ointments, alcohol, brilliant green or iodine to the injured area, especially for 3rd and 4th degree burns. It is enough to cover the wound with a sterile cloth to prevent further infection.
At high temperatures, the tissue at the burn site can melt and stick to the burned skin. There is no need to try to remove it, since trying to separate it from the body can further injure the burned areas. Also, when providing first aid (First Aid), you should never puncture the resulting blisters, which can lead to inflammatory processes.
To prevent burn shock and to replenish lost water balance, you can give the patient a large amount of fluid. This rule does not apply if the victim experiences nausea or vomiting.
Emergency assistance is required for the victim in the following cases:
- loss of consciousness;
- pallor;
- increased heart rate;
- a sharp decrease in blood pressure;
- breathing problems;
- the presence of burns exceeding 20% of the skin surface (for older people and children this figure is reduced to 10%);
- burns associated with electric shock or chemicals.
If at least one sign is present, the victim should be immediately taken to a medical facility to provide qualified medical care.
Degree of tissue damage
In total, there are four main degrees of thermal burns, with the first and second being considered superficial, and the third and fourth being deep (Figure 3).
The severity is determined by the area of the lesion and the injured layers of the epidermis:
- First degree:
accompanied by redness and swelling of the damaged area. The skin starts to hurt. The burning sensation and pain are especially strong when touched. As a rule, the complete healing process does not take more than 5 days. - Second degree:
This type of burn occurs as a result of prolonged or sudden exposure to high temperatures. In addition to redness and swelling of the area, blisters with a cloudy yellow liquid inside appear. They protect the affected skin from external influences and promote the formation of new skin, so such blisters should never be opened. - Third degree:
occurs with very prolonged exposure to hot substances on the skin. A characteristic feature is the formation of dry or wet tissue necrosis. Healing occurs through scarring and takes a long time. - Fourth degree:
the most terrible type of injury, since it is often accompanied by damage to a large area of skin. The skin color turns black and the blisters may coalesce. In this case, necrosis occurs not only of the epidermis, but also of tissues, tendons, and sometimes bones. This condition requires emergency medical care, as it threatens the life of the victim.
Figure 3. The degree of burn is determined by the area and depth of tissue damage.
This classification of the degrees of thermal burns is used mainly by doctors, but ordinary people should also know this information in order to develop a clear algorithm of actions. This will help provide first aid to the victims before doctors arrive.
First aid rules
In most cases, tissue damage under the influence of high temperatures occurs as a consequence of a fire or accident. Therefore, first aid to the victim always begins with stopping the contact of the skin with the source of the pathological condition. In simple words, you need to extinguish the clothes, take the person out of the danger zone. Sticky clothes should not be torn off. It is better to cut the fabric with a sharp knife or scissors.
The next step in providing first aid to a thermal burn victim is applying a bandage. It is important that the tissue is dry and aseptic. The best option is a bandage or gauze. If you don’t have dressing materials at hand, you can use any cotton fabric (pre-treated with an alcohol-containing liquid or ironed).
In case of severe thermal burn (3-4 degree), it is important to avoid painful shock. It is necessary to place the victim in a horizontal position, cover him (severe hypothermia is possible), and give more fluid. If possible, narcotic painkillers (morphine, promedol) should be administered intravenously.
Symptoms of thermal burns
Symptoms of a burn directly depend on the area and depth of the lesion. Each stage has its own characteristics, so before making a diagnosis, doctors must conduct a full examination of the patient (Figure 4).
Thermal burns are especially dangerous for a child, who tolerates pain much worse, and it is more difficult for a fragile body to cope with complications. That is why even the first degree of injury in children is a reason to go to the hospital.
It is impossible to confuse a burn with any other injury. The affected area first becomes red and swollen, and the person feels severe pain and burning. In the second stage, these symptoms intensify and are accompanied by the formation of blisters.
Figure 4. The severity of symptoms depends on the degree of injury
At the third stage, necrosis occurs, and at the fourth stage, tissue charring occurs, since the deep layers of the epidermis and the tissues located underneath are affected. In addition, one should not lose sight of the fact that such an injury may be accompanied by complications, but we will discuss them below.
Human skin structure
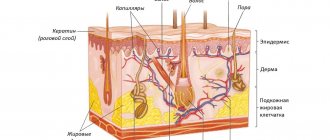
The skin is the border between our body and the external environment. Consists of water, protein, inorganic compounds and fatty acids. Despite its small thickness, it makes up about 16% of the total mass of the human body, which is about two square meters. It contains several layers.
Epidermis
The outermost layer of skin, which is formed by epithelial cells. Thickness – up to 2 mm. The thickest layer is located on the skin of the feet, the thinnest is on the skin of the genitals and eyelids. They are horny cells that act as a barrier to the penetration of pathogenic flora into the skin.
Dead cells are removed by washing or using special scrubs. In their place, new similar cells immediately appear from the deep layers of the epidermis. This process is constant and endless.
The epidermis consists of five layers. It is nourished by intercellular fluid coming from the dermis.
Dermis
Elastic tissue that is the base or framework of the skin. The thickness of the dermis varies up to 5 mm. The thickest skin is on the shoulders, back and hips. It consists of a papillary layer located under the epidermis and a deeper reticular layer.
The papillary layer contains numerous papillae or outgrowths with capillaries, nerve endings and hair follicles located in them. There are many papillae on the skin of the palms, soles and fingers.
They are practically absent on the skin of the ears and forehead. The papillary layer retains heat in the body, provides tactile sensations (cold, warmth, pain), and provides an individual fingerprint pattern due to the different heights of the papillae. It also affects hair thickness and growth.
Under the papillary layer, on the hypodermis, there is a reticular layer of the dermis formed by loose connective tissue. It does not have a sharp border with the lower layer - the hypodermis: it merges smoothly into it.
The reticular layer contains blood and lymphatic vessels, sweat and sebaceous glands. As well as collagen fibers and elastin. This layer provides skin nutrition, elasticity, firmness, regulates sweating and the function of the sebaceous glands.
Subcutaneous fat
She is also a hypodermis. It is the lowest layer of skin. It consists of fatty formations and loose connective tissue, richly supplied with blood and lymphatic vessels, as well as nerve endings.
The thickness of the layer depends on age (decreases with age), gender (more in women), bad habits, nutrition and lifestyle (with a sedentary lifestyle, this layer is thicker). Most fat is located on the buttocks, abdomen and chest.
There is no fat at all on the eyelids, as well as on the tip of the nose. This layer regulates heat exchange, promotes figure shaping, reduction of wrinkles and skin mobility. It also softens shocks coming from the outside and is a repository for vitamins. The fat layer contains the hormone leptin, which is responsible for the feeling of fullness and appetite.
Treatment
Treatment of patients with serious thermal burns is carried out in a hospital setting. If the lesion belongs to the first or second stage, after examination by a doctor the patient will be sent home and treatment will have to be continued at home (Figure 6).
At home, dressings with special wound-healing ointments and creams are usually used. The use of folk remedies is undesirable, as they can only worsen the situation.
Back at the hospital, doctors clean the wound. Since the burns are very painful, the procedure is performed under anesthesia. The skin around the wound is treated with an antiseptic, and the affected area itself is cleaned of contaminants.
Further treatment depends on the stage of the burn. At first, an antiseptic treatment is sufficient, followed by applying a bandage with an antibacterial cream (Levomekol, Betadine, Levosin). If the burn is of the second degree, dressings are carried out every 3-4 days, although the same drugs are used.
Figure 6. Only minor 1st and 2nd degree burns can be treated at home
Patients with third and fourth degree burns must be hospitalized, and wet bandages with antiseptics are changed every two days. Treatment at home for such lesions is not provided.
Description and causes of damage
What is a thermal burn?
According to experts, this injury is damage to the skin and mucous membranes under the influence of high temperatures. Thermal burns can be caused by solid, liquid and gaseous substances characterized by high temperatures. Heat injury is a common household injury. You can get injured when cooking food, scalding with boiling water, touching hot objects, as well as under the influence of steam, fire flame and light radiation.
Assessing the affected area
To choose the right treatment tactics, it is important to assess the damaged area. Approximately, all burns are conventionally divided into non-extensive - up to 10% of the body is affected, and extensive - over 10%.
- Minor burns cause a general pain reaction, sometimes with fever and headache, a feeling of discomfort and pain in the area of damage;
- With extensive lesions, more serious complications and disruptions in the functioning of the entire body are observed - burn disease.
There are several effective, simple techniques that will help assess the affected area. The most popular techniques are the “rule of nines” and the “rule of the palm.” Of course, they give an approximate, not exact picture, but they are easy to use and quite effective.
Rule of nines
In 1951, scientist Wallace proposed a rule according to which the adult body is conditionally divided into zones whose area is 9 or 18 (2 to 9)%. Thus, the following zones are distinguished:
- 9% are head and neck;
- Front torso – 18%;
- Back torso – 18%;
- Hand – 9%;
- Leg – 18%;
- Groin and perineum – 1%.
This proportionality is typical for adults. In children, the head and neck make up 21% of the total body area.
Palm rule
In 1953, Glumov proposed a simpler method, which is also related to percentages. Only the palm is taken as a measurement, which occupies approximately 1% of the body area of an adult. So, using the palm of your hand, you can determine how many percent of the body is affected.
If large areas are affected, even with a superficial form, death cannot be ruled out. How dangerous thermal burns are to life is usually calculated using a special formula. To do this, the percentage of the affected body area is added to the patient's age.
- The forecast is considered favorable if the amount is less than 60;
- Relatively favorable – from 61 to 81;
- Doubtful - from 82 to 100;a
- Unfavorable – over 100.
Another method for predicting survival is also used, which sums up the percentage of superficial lesions and triple the percentage of deep burns.
- If the total is 35% or higher, then it is not always possible to help patients - medicine is powerless.
While it is not difficult to recognize a thermal burn, it can be difficult to determine how deeply the tissue is damaged and to identify the exact area of damage in the first hours and even days. The picture becomes clearer on days 3–4, when the depth of the affected tissue becomes noticeable and the contours of the injury emerge.
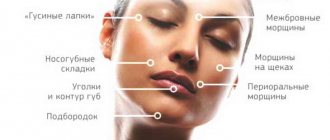
Danger zones: burns of the face, neck, chest
Injuries to the upper half of the body are considered the most dangerous, since damage can affect important functional organs: the respiratory tract, eyes, ears.
A burn to the chest, as a rule, spreads to the neck area, which can lead to difficulty breathing; increasing swelling prevents the passage of oxygen through the respiratory tract. In case of deep tissue damage in these areas, emergency necrotomy is performed in order to prevent the development of a fatal complication.
With thermal damage to the face, the pain syndrome is most pronounced, and a strong reflex closure of the eyelids also occurs, which, as a rule, prevents damage to the conjunctiva. Swelling of the eyelids and blepharospasm greatly complicate the diagnosis of corneal damage, so such burns must be observed by a doctor.
In case of contact with an open flame, injury to the conducting respiratory tract poses a great threat.
Symptoms of damage in this case will be:
- singed nose hairs,
- swelling of the mucous membrane,
- difficulty breathing,
- dry cough,
- burning sensation when breathing.
Burns in these areas are considered severe and require specialized treatment, so if you receive them, you should immediately consult a doctor.