What is impetigo and how to treat it? Impetigo is a contagious skin disease caused by staphylococci or streptococci, sometimes a combination of both. The disease affects the upper layers of the epidermis and externally manifests itself in the form of multiple pustular rashes, turning into scabs with crusts. Most often, children attending child care institutions are susceptible to the disease. For adults, the likelihood of becoming infected is also possible, especially with a low level of personal hygiene.
Infection occurs through microtraumas - scratches, bites, cuts and abrasions. When pathogenic bacteria come into contact with a damaged layer of skin, they actively multiply, causing inflammation. Such microorganisms are always present on the surface of the skin, but with hygiene and regular washing, their number is significantly reduced and cannot cause skin diseases.
Causes
The main reasons, as a result of which impetigo begins to progress:
- non-compliance with sanitary and hygienic rules;
- weakened immune system;
- diabetes;
- formation of abrasions, bites, microcracks on the skin;
- hot climate (hot or humid);
- presence of foci of infection in a family member.
The main risk group includes people in the following categories:
- people who often visit public places - saunas, swimming pools, showers;
- children under 6 years old;
- who have suffered severe infectious or dermatological diseases.
It should be noted that the development of a pathological process is only possible if a person’s immune system is too weakened.
Classification of impetigo
In dermatology, it is customary to classify impetigo (see photo) depending on the cause of the disease and clinical manifestations. There are:
1. Streptococcal (contagious) impetigo: the cause is streptococcus, which most often affects the skin of children and women. A very common and contagious form of impetigo.
Includes several varieties:
- Ring-shaped impetigo is a type of streptococcal type and is characterized by the appearance of large grouping conflicts. Their central part dries out, forming a crust, and new conflicts appear on the periphery, forming ring-shaped figures. This type of disease most often affects the feet, legs, back of the hands and the nail fold area.
- Lichen simplex (“dry” pyoderma) – occurs on the face of children and is considered an abortive form. It manifests itself clinically as erythematous pink spots with peeling. The elements resolve under sun exposure, leaving persistent depigmentation;
- Slit-like impetigo (jam) - develops in people who sleep with their mouths open, through the corners of which saliva passively flows, as well as in those who have the habit of licking their lips. It is clinically manifested by a rash of pustules in the corners of the mouth, at the wings of the nose, and outside the palpebral fissure. Pustules erode in the form of a slit-like defect in the skin and mucous membranes. The surrounding skin is tense, painful, and difficult to epithelialize, since lip movements break thin epithelial films;
- Bullous impetigo - manifests itself in the form of two-centimeter blisters with a dense tire, filled with cloudy exudate mixed with blood. The process is complicated by the appearance of swelling around the affected area, as well as an increase in temperature, headache, and weakness. A particularly severe course of the disease is observed in pre-existing skin diseases.
- Syphiloid impetigo is a disease noted in newborns. A distinctive feature is the rash of phlyctenas on the buttocks and in the subgluteal area. Phlyctenas open, forming erosions with an infiltrated base, resembling chancre, and are resolved by the formation of crusts that leave no trace behind;
- Vegetative impetigo - the disease is characterized by spontaneous spread of bursting blisters with the formation of erosions covered with purulent crusts;
- Impetigo of the mucous membranes - a rash of aphthae in the oral cavity, on the mucous membranes of the cheeks, gums, tongue, nasal passages, mucous membranes of the eyes;
- Intertriginous streptoderma - rashes are localized in large folds of the skin, where, due to aseptic conditions (sweat, weeping), continuous itchy and painful erosive surfaces with a halo of remaining epidermis along the periphery are formed. The boundaries of the lesion are clear, there is a tendency to peripheral growth.
2) Staphylococcal impetigo (ostiofolliculitis, Bockhart's impetigo) - occurs in men, children, and adolescents. Occurs at the mouths of hair follicles when the rules of basic cleanliness are not followed. If it persists for a long time without treatment, it transforms into a carbuncle. Available in two versions:
- Non-bullous form (superficial folliculitis) - caused by white staphylococcus, characterized by small (1.5 mm) purulent blisters, has no tendency to spread, the primary elements quickly dry out into crusts, which, falling off, leave no trace.
- Bullous form (deep folliculitis) - it is caused by Staphylococcus aureus. It manifests itself in the formation of a nodular-vesical rash (5 mm) around the hair follicles, the primary elements become denser, tend to penetrate into the deep layers of the skin, the vascular bed, therefore, in the clinic there are symptoms of intoxication, and the outcome of the process is a scar.
3. Mixed impetigo (vulgar impetigo) – occurs when streptococcal impetigo is complicated by staphylococcus, when the appearance of conflicts is accompanied by itching, scratching, and the addition of a secondary infection. The rashes are multiple, covered with thick crusts, localized in the face, neck, joints, near the nipples of the mammary gland, and on the genitals. Bullae and erosions are painful, tend to spread (through a dirty towel, bed linen), and regional lymph nodes are involved in the process.
The body protects itself
Impetigo is caused by bacteria of the streptococcal or staphylococcal series. There are types of infectious rash caused by both groups of microorganisms at the same time. Staphylococcus or streptococcus bacteria are found on the skin of adults and children. But pathogenic microorganisms do not always lead to the development of this disease.
The skin is a barrier through which a pathogenic infection cannot penetrate into the deeper layers of the skin and cause inflammation. When washing, most of the virulent microbes are washed away with water along with the stratum corneum of the epidermis. The mucous membranes are protected by ciliated epithelium, which removes microbes from the surface. Human immunity also plays an important role in preventing the development of the disease.
It maintains an optimal pH level of the integument, which blocks staphylococcus and streptococcus. Normally, the body protects itself from pathogenic microbes, but when accompanying factors appear, this pathology develops.
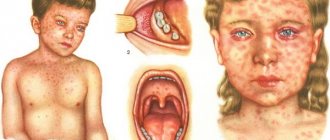
Impetigo in children
Impetigo in children manifests itself in the formation of red spots that turn into scabs in the form of crusts. First of all, they become noticeable in the mouth, nose, behind the ears, and on the back of the hand. Conflicts sometimes occur on the gums, which causes the child a lot of inconvenience and pain. Children often experience rashes in the corners of the mouth, so-called jams.
Thin-skinned blisters burst, forming slit-like erosion. A crust quickly forms in its place. Long healing of wounds in children is the result of the habit of licking the corners of the mouth. Staphylococcus and streptococcus bacilli enter the child's body through insect bites, abrasions and other damage to the skin, in contact with other children. This applies most to children attending preschool institutions.
Clinical manifestations
Symptoms of impetigo (see photo below) are mainly associated with an infectious pathogen. However, characteristic of all of them is a superficially located primary element - phlyctena, which is a pustule formed under the epidermis and filled with light, cloudy or purulent contents, sometimes mixed with blood.
Histological examination reveals leukocytes, a small number of lymphocytes and fibrin elements in the phlyctene. There is also an accumulation of inflammatory fluid in the intercellular space of the spinous layer of the skin, and in the upper layers of the dermis there is a slight inflammatory infiltrate with leukocytes and lymphocytes.
Depending on the causative factor, the following types of impetigo are distinguished:
- Streptococcal, or superficial streptoderma, contagious impetigo, Jadassohn's impetigo, Fox's impetigo.
- Staphylococcal, or superficial staphylococcal ostiofolliculitis, Bockhart's impetigo, follicular impetigo.
- Mixed, or vulgar, strepto-staphylococcal.
Development mechanism
The nature of the clinical picture largely depends on who is the causative agent of the infection. However, there are general symptoms that allow a preliminary diagnosis to be made. This is a superficially located phlyctena - a pustule that forms under the epidermis. It is filled with purulent contents. Histological examination allows us to detect the presence of leukocytes, lymphocytes and fibrin elements. Under the phlyctena in the spinous layer of the skin, an accumulation of inflammatory fluid is observed in the space between the cells; a small infiltrate is formed in the upper layers of the dermis.
The appearance of other signs of pathology largely depends on what caused the development of the purulent-inflammatory reaction. The following table helps you see the most complete picture of possible manifestations.
| Types of pathology | Pathogen | Affected area | Nature of skin defects |
| Staphylococcal impetigo (ostiofolliculitis) | Staphylococcus aureus | Skin of the face, neck, forearms, thighs, legs. Pustules can be grouped or appear on different parts of the body | The hair follicle becomes inflamed. First, redness appears at the site of the lesion, then compaction, which upon palpation exhibits severe pain. Then a small abscess appears, the diameter of which does not exceed 2 mm. Its surface rises slightly above the epidermis, and pus is clearly visible under the thin skin above it. The tissue around the abscess is red. The abscess opens after a few days, the pus bursts out, revealing a shallow wound underneath. It becomes crusty over time. When it falls off, a pigmented spot remains. |
| Bullous impetigo | Staphylococcus aureus | The back surfaces of the hands, less often the area of the lower leg and feet | Large ulcers up to 3 cm in size appear. After opening, an open ulcer forms in their place, which increases in size over time. Bullous impetigo lasts longer than other forms of infection |
| Slit-like impetigo (jam) | Staphylococcus aureus | In the corner of the mouth, where the upper and lower lips meet | One small bubble forms exactly at the junction. When the pus in it matures, it opens, and in its place a honey-yellow crust appears. The process of abscess formation is accompanied by itching and profuse salivation. Eating becomes painful. The habit of licking lips is a factor that contributes to the transition of the acute phase to the chronic phase. Very often, crevice impetigo appears in case of a lack of vitamin B in the body, as a complication after rhinitis, conjunctivitis, dental caries |
| Lichen simplex is a dry type of streptococcal impetigo, in which there are no purulent-inflammatory reactions | Staphylococcus aureus | Skin around the mouth, on the cheeks and chin, on the torso, arms and legs | White spots appear, which are clearly visible against the background of healthy skin. They have a round or oval shape, clear boundaries, and peeling occurs inside them. Severe itching occurs at the affected areas. When exposed to sunlight, the spots disappear, but the skin underneath does not tan. |
| Impetigo of the nail fold | Staphylococcus aureus | The surface of the nail plates on the sides | Small bubbles appear on the side of the nail fold, containing a clear liquid inside. Gradually their cavity fills with pus. Pain occurs and the skin around the lesion swells. When the blister opens, erosion forms and spreads to the nail. The affected area is shaped like a horseshoe. After the wound heals, rejection of the nail plate becomes possible. In people with immunodeficiency conditions, this form of impetigo is especially severe, it causes inflammation of regional lymphatic vessels, increased body temperature, and a general deterioration in well-being. |
| Contagious streptococcal impetigo | Streptococcus | Face, sides of the body, skin of the arms and legs | It begins with the appearance of a small red spot; after a few hours, a bubble with a diameter of up to 3 mm forms in its place. It contains transparent contents, over time it becomes cloudy, the elasticity of the pustule decreases, it becomes flabby, and then opens on its own. After the eruption of pus, a gray crust forms. When it falls off, a pink spot with a bluish tint remains on the skin. The process of suppuration lasts three to four weeks |
| Ring-shaped | Streptococcus | It always starts acutely; small, flat-shaped bubbles appear on the body, filled with cloudy contents. They constantly increase in size due to growth towards the periphery. Then they dry out. The process starts from the center. A crust similar to a plate is formed. It has a yellow-brown color. The shape of the crust gives the form of pathology its name | |
| Streptococcal diaper rash | Streptococcus | Where there are large folds. In women under the mammary glands, in obese people, where two areas of skin are in close contact with each other. In small children, in the armpits, in the crease between the buttocks, behind the ears, in the folds of the abdomen | First, isolated bubbles appear, the diameter of which does not exceed 2 mm, then they merge, open, and in their place a large erosion appears, having a bright pink color. It is characterized by constant weeping. Over time, a new area of affected skin appears near the main lesion. Wetting leads to cracks. They cause severe pain. Against this background, there is a deterioration in the general condition |
| Vulgar impetigo (mixed type of infection) | Both staphylococci and streptococci | Skin around the mouth, eyes and nose | First, infection occurs with streptococci. Their invasion causes redness of the skin, it swells, and then a bubble with cloudy contents appears in this place. When it bursts, an ulcer opens. It promotes the penetration of Staphylococcus aureus. At the same time, you can see the formation of various kinds of ulcers on the skin. After opening some boils, a golden crust forms; after opening others, crusts of a darker color form. Different pustules have different maturation periods. This phenomenon helps to differentiate the form of the disease |
| Bockhart's disease | Staphylococcus | Scratching areas on the back of the hands | Large pustules appear, up to 1 cm in diameter. The pathology is a complication of scabies and develops after the addition of a bacterial component |
Streptococcal impetigo
This type of disease most often affects young women, adolescents and children. It is characterized by the appearance of red spots, which transform after a few hours into scattered or grouped elements that tend to grow peripherally and are capable of merging with each other. If left untreated, they occupy fairly large areas of skin.
Phlyctenas range in diameter from 2 to 10 mm, are surrounded by a halo of hyperemia (redness), have a thin flabby covering and contain a cloudy liquid. Most often, rashes are localized on the skin of the face (mask-like impetigo), less often - on the skin of the legs, hands and feet.
When the primary elements are opened, a juicy bright pink erosive surface is exposed. As a result of the evolution or opening of conflicts, their contents or discharge shrink into thin crusts of light yellow or grayish color. The latter disappear within 3-7 days, and in their place remains a pinkish or temporarily depigmented area covered with a thin layer of epithelium. This lesion is surrounded by exfoliating horny epithelium in the form of a narrow “collar”.
Symptoms
The rate of development of impetigo is quite high, the incubation period of the disease does not exceed a week. And the first symptoms may appear even earlier, 3 to 5 days after pathogenic cocci penetrate the skin cells.
Each type of impetigo has its own characteristic symptoms, but there are also general signs of the disease.
Most often, rashes are localized on exposed parts of the body , on the face, especially in the nose, around the mouth or eyes, as well as on the extremities:
- The affected areas experience itching, pain, and burning.
- Inflammation of the lymph nodes occurs.
- Hyperthermia is observed, that is, an increase in body temperature.
The development of impetigo occurs in several stages:
- first - the appearance of red spots on the skin, then blisters (phlycten) with liquid contents, which contain pus. There is an area of inflammation around the conflict;
- when the blisters burst, they turn into sores;
- then the formation of yellowish crusts (scabs) begins;
- After a few days, the crusts fall off, these areas of the skin often have a pink color.
With impetigo, the rashes are scattered or crowded. The rate of development of painful lesions depends on how weakened the patient’s immunity is.
Rapid damage to the skin occurs when the body's defenses are significantly weakened.
The symptoms inherent in each type of impetigo will be discussed later in the article. The specific manifestations of the disease depend on its form and the type of pathogen.
Staphylococcal impetigo
Staphylococcal impetigo (bullous), known as folliculitis, develops when bacteria enter the pores of the skin and where hair grows. Pus immediately forms in these places. Most often, children aged from birth to two or three years are susceptible to this type of disease. The disease affects the child's limbs, back or abdomen.
The disease can be diagnosed as follows: with superficial impetigo, many red spots appear on the body, which are separate from each other and almost invisible. After some time, each spot turns into a bubble filled with pus, from which a hair sticks out. At the third stage, the bubble bursts and forms a honey-yellow crust.
In the second case, if the infection has penetrated deeply, then purulent formations appear on the skin. They can reach one centimeter in diameter, the skin around the abscess turns red, and the abscess bursts after a couple of days. Impetigo infection at this stage is very dangerous for children; scars and welts may remain on the skin, even if treatment was carried out on time.
Definition
Streptococcal impetigo (ICD 10 L01) is a highly contagious skin disease caused by streptococcal bacteria. It manifests itself as phlyctenes (fine blistered rash) with swelling and redness. Arranging in groups, the blisters merge and enlarge, and after the rash goes away, pinkish spots still remain on the skin for some time.
Skin manifestations renew every five to six days. The infection quickly spreads to healthy areas and the process begins again. Improper treatment and prevention can cause damage to a large area of skin. The most common location: face, hands, shoulders and other open areas of skin.
In dermatology, the following types of streptococcal impetigo are distinguished: bullous, ring-shaped, slit-shaped, as well as tourniol (disease of the nail folds), streptococcal intertrigo and post-erosive syphilide.
Vulgar impetigo
Usually occurs in children. It has a high degree of contagiousness. Characterized by the appearance of blisters of streptococcal causes. As a result of the addition of a staphylococcal infection, the light contents of the bladder acquire a thick consistency and a yellow color. The contents of the conflict tend to quickly dry out into thick crusts of a yellowish-green color that look like lumps. Beneath them a weeping erosion surface is revealed.
Usually the number of rash elements is large, they are accompanied by itching, and tend to quickly spread throughout the body and merge with each other. The predominant localization is the face and open areas of the limbs. In the presence of pediculosis, the rashes are localized mainly on the scalp, in case of scabies - in the elbows (Hardy's symptom), inner thighs, on the penis and in the buttock area. Often recurrent rashes occur in the area of the wings of the nose, ears and eyelids against the background of infectious and inflammatory processes (blepharitis, rhinitis, otitis).
With the rapid progression of the process with the spread of rashes throughout the body and the presence of a large number of elements with an erosive surface and papular infiltrate, symptoms of general intoxication are noted in the form of a slight increase in temperature, headache, weakness, general malaise, lack of appetite, and sleep disturbances. In more severe cases, complications are possible - severe intoxication, high body temperature, focal erythroderma, lymphadenitis and lymphangitis, abscesses and phlegmon, kidney damage in the form of acute glomerulonephritis. [adsen]
Complications
Mostly impetigo goes away without dangerous consequences. But sometimes this disease can cause permanent harm.
Streptococcal impetigo can lead to disruption of the body's protective function, resulting in damage to the kidneys or heart.
After a viral infection, a person may develop nephritis, myocarditis or rheumatism. The staphylococcal species is capable of reproducing in the deep layers of the skin, which can cause a purulent inflammatory process.
Thus, you should not ignore the symptoms of the disease. If obvious signs are detected, you should immediately consult a doctor to prescribe antibacterial or local therapy. Be healthy!
Diagnostics
The diagnosis may be suspected already during the initial examination. The doctor clarifies the nature of the primary rash and the characteristics of the course of the disease. Additional research methods include dermatoscopy. Bacteriological examination - culturing the discharge on nutrient media - helps to completely confirm the diagnosis.
In case of recurrent impetigo, to diagnose this disease, the patient is recommended to study the immune status, which helps to determine disorders in the immune system.
Other skin diseases occur with similar symptoms: Dühring's dermatitis, pemphigus of newborns, simple contact dermatitis. A dermatologist will help you distinguish these diseases from each other.
How to treat impetigo?
The main treatment for impetigo is local. These are antibacterial ointments (tetracycline, erythromycin), aniline dyes (brilliant green solution, fucarcin), alcohol solutions (salicylic alcohol), vitamin therapy. In severe cases, they resort to oral antibiotics.
Recommendations for patients with impetigo:
- The patient must have his own separate towel, dishes, and personal hygiene items.
- Do not wash: while washing in the shower or in the bath, especially if you rub your body with a washcloth, the infection spreads across the skin.
- The apartment where the patient is located must be wet cleaned daily with disinfectants.
- If a child gets sick, it is necessary to isolate him from the group in kindergarten: due to the immaturity of the immune defense, the infection spreads faster among children.
- It is recommended to eat more foods containing vitamin C: lemons, sauerkraut, cranberries, etc.
- You should avoid eating sweets. Sugar is a nutrient medium on which streptococci and staphylococci multiply well.
Treatment and folk remedies are widely used. For example, during this period of time, an alcoholic tincture of calendula is sold, which is used to wipe the lesions of impetigo. The alcohol itself and the calendula itself have antibacterial properties. They also take tinctures of chamomile, string, St. John's wort... In a word: “Everything is possible, but under the supervision of a doctor.”
Risks for the sick person
With timely and proper treatment, impetigo goes away within 2-4 weeks.
An increase in the area of the lesion occurs due to self-infection during scratching. Pus from the burst blisters, containing a huge amount of streptococci, flows out of the burst pustules, and when scratched, spreads throughout the body.
However, you should be aware that complications can occur:
- With recurrent forms of contagious impetigo, rheumatism may occur - a serious and practically incurable disease.
- Children may develop scarlet fever, because it is nothing more than a generalized streptococcal infection.
- A complication occurs in the form of glomerulonephritis - an autoimmune inflammation of the kidneys.
- In severe cases, sepsis – blood poisoning – is possible.
Traditional methods of treating impetigo
Some patients actively use traditional medicine to get rid of unpleasant symptoms of skin diseases, among which the following recipes are the most famous:
- comfrey grass is crushed and brewed with boiling water, after which it is left for 7-10 minutes to infuse. After cooling, it is recommended to treat inflamed areas of the skin with the solution;
- you need to take equal amounts of chamomile, horsetail and elecampane root, calendula, plantain and St. John's wort. The prepared mixture of medicinal herbs should be poured with boiling water (1 liter) and boiled for 10-15 minutes. After cooling, the solution is filtered and taken ¼ cup before meals;
- to dry the blisters, you can use powder from the spores of the club moss, which is sprinkled on the affected area;
- flaxseeds are poured with cold water and boiled over a fire for 5-7 minutes, after which the solution is cooled, filtered and applied as a lotion to the affected areas;
- For internal use, it is recommended to prepare a decoction of alder cones, chamomile flowers, aralia roots, licorice, leuzea and kopeck. All ingredients are crushed, poured with water and kept on fire for 5 minutes, after which they are filtered and taken orally, 1/3 cup before meals;
Despite the widespread use of traditional medicine recipes in the treatment of impetigo, doctors are ambivalent about this method of getting rid of negative manifestations, arguing that prevention plays the main role.
Prevention
Certain rules must be followed:
- Activities aimed at strengthening the immune system. An active lifestyle, exercise, and sufficient exposure to fresh air - all this reduces the risk of not only impetigo, but also any infections.
- Careful personal hygiene. Skin contamination is one of the factors that increases the risk of developing streptococcal and staphylococcal infections.
- Complete nutrition. The human body must receive daily all the substances necessary for the normal functioning of the immune system.
- Compliance with occupational hygiene rules. Especially in those organizations where workers often experience injuries to the skin of their hands (scratches and cuts), where they are constantly in contact with various fuels and lubricants.
- Isolation of the patient, frequent wet cleaning with disinfectants. This will help avoid infection. The risk is especially high among people with reduced immunity: children, the elderly, pregnant women.