Eczema is an inflammatory process that affects the skin on the hands. The disease has several causes, but most often occurs against the background of frequent allergic reactions.
Eczema affects people of all ages, including children. Although the disease is not dangerous, it brings severe discomfort to the patient due to its unpleasant appearance. There is also a danger of the disease becoming chronic.
It is very important to consult a dermatologist at the first symptoms; the doctor will be able to determine the cause of the disease and prescribe the necessary therapy. Establishing the exact cause is the key to effective treatment.
Varieties and atypical forms
To begin with, eczema (translated from Greek “ἐκζέω” - “boil”) itself is an atypical manifestation, an abnormal reaction of the body to something. Therefore, they are all atypical to one degree or another. It is quite difficult to structure eczema into types, since there are often two or more forms, plus one can cause the other.
In general it goes something like this:
- Endogenous eczema. Includes true (idiopathic, systemic), dyshidrotic, seborrheic, tylotic (horny, callous), varicose eczema. It is characterized by the fact that it is triggered by internal factors.
- Exogenous eczema. Includes bacterial, viral, mycotic (fungal), allergic (subspecies - occupational), sycosiform eczema. It is clear that here the disease developed as a result of exposure to some external agent.
- Children's eczema is considered separately, since in a child's body it is even more difficult to distinguish the etiology than in an adult.
But such a classification remains largely arbitrary. For example, some kind of endogenous eczema is caused by malfunctions within the body. But these failures, in turn, as a rule, also turn out to be a consequence of external influences. For example, a traumatic combination of poor ecology, unhealthy lifestyle and cold climate.
Other classifications divide eczema by localization and symptoms, but this approach is quite superficial, since eczema provoked by completely different factors can have similar localization and manifestations.
Main article: Types of eczema
How to treat the disease?
An experienced doctor knows how to treat eczema and has the right to prescribe treatment and choose a way to get rid of the disease. Self-medication is contraindicated: having noticed the first symptoms, it is better to immediately go to the hospital, get tested and get recommendations from a specialist. Based on the results of tests and diagnostics, the doctor chooses a treatment method. The patient must be prepared for the fact that the therapeutic course will last a long time. Much depends on the patient himself: going to the hospital in a timely manner, following a special diet developed by a doctor, taking medications regularly, etc.
Treatment of any type of disease is prescribed strictly individually for each patient, who, if side effects occur, must immediately report them to the doctor.
This or that type of eczema on the hands, depending on the cause and treatment, goes away in children and adults over different periods of time. What matters is the patient’s age, his state of health, the presence or absence of bad habits, active lifestyle, and diet.
How to treat eczema on hands? First of all, the doctor prescribes a comprehensive medication regimen. First, the dermatologist will prescribe drugs of a pathogenetic nature, which should block the influence of external factors and dysfunction of internal organs. The next step will be nonspecific therapy:
- blood transfusion;
- hirudotherapy;
- autohemotherapy;
- lactotherapy.
If the form of eczema is severe, then treatments such as:
- Hemosorption.
- Plasmapheresis.
- Enterosociality.
- Taking biostimulants (injections containing aloe or placenta extract).
If the disease provokes the development of neurotic disorders, then the doctor will definitely prescribe the use of Sodium bromide, Bromcamphor and tranquilizers. Additionally, sedatives are prescribed, which should help the body cope with intoxication and reduce the influence of toxins and harmful substances.
Often the disease affects the areas between the fingers, which forces the dermatologist to prescribe hormonal medications. The course of treatment with hormones cannot be long, but must be supervised by a doctor. You cannot prescribe or cancel hormones on your own, so as not to harm the body. Drug therapy is accompanied by mandatory intake of vitamin complexes of groups E, B, folic and ascorbic acids. The complex therapy includes the following components:
- Antihistamines, which are prescribed as injections, tablets or solutions.
- Immunomodulators.
- Stimulants.
- Enzymes.
- Probiotics.
- Antibacterial drugs.
- Antifungal agents.
- Local antimycotics (ointments and creams).
Causes
Modern dermatology, immunology and allergology, when studying cases of eczematous lesions, no longer consider the causes of the development of the disease separately. There is always a complex of reasons in which one of them simply becomes a trigger. For example, not all people have staphylococcal infections that cause eczema, but for some it becomes the “spark” that ignites the prepared “fuel” (a complex of associated factors). It is still unclear whether a genetic predisposition is necessarily required, or whether eczematous inflammation can develop in a person who was not initially prone to it at all. The disease is chronic, varying greatly in the frequency and intensity of relapses.
The main set of factors that create conditions for the onset of the disease are as follows:
- Genes encoding the structure of cell membrane receptors (a type of antigen). It has been confirmed that isoantigens on blood cells can be a concomitant or provoking factor. It was revealed that among patients with eczema, the majority are carriers of isoantigens A, M, N, found on the blood cells of patients. The exact mechanism of action linking isoantigens and changes in the immune system is not fully understood.
- The immune changes themselves during the development of eczema are generally known. This is an inhibition of the activity of T-lymphocytes, an abnormally high activity of B-lymphocytes. Their accelerated transition into plasma cells, which synthesize the main allergenic immunoglobulin E. Along with Ig E, the concentration of Ig G in the blood is increased, which normally begins to be actively released during infection, but can also occur when the body reacts excessively to subthreshold doses of bacteria or viruses . But Ig M, on the contrary, is lowered, because is produced in immature B-lymphocytes, the number of which is also small in eczema.
- According to the latest data, it is clear that it is incorrect to talk about weakened immunity as a cause of eczema. No, the situation here is rather the same as with autoimmune diseases. He simply becomes inadequate. According to one theory, due to the mentioned shifts, immunoglobulins begin to attack the body's own cells. In this case, skin cells.
- For a long time, it was believed that eczema was neurological and/or mental in nature. As one of the factors, of course. Damage to the peripheral nerves of the extremities, for example, with polyneuropathy, has been more than once noted with the subsequent development of skin inflammation. The connection between the psyche and the development of skin inflammation has been studied to an even lesser extent. Perhaps the mental factor somehow turns into a neurological one.
- For example, the functioning of the autonomic nervous system is disrupted, and this leads to disruptions in the functioning of the endocrine glands and metabolism.
- Persons with a tendency to eczematous inflammation often encounter it if they become ill with some kind of infection: staphylococci, herpes viruses, Candida fungi, helminthic infestations.
- Individual allergic reactions often lead to eczema. For example, allergic contact dermatitis can develop into eczema.
- Autoimmune diseases are of particular importance. For example, gastrointestinal tract (UC, Crohn's disease). An immune failure has already occurred in the body, so the formation of autoantibodies to cells of other tissues is facilitated.
- A complex set of external conditions: unhealthy diet high in trans fats (fast food), unfavorable environmental conditions (long-term exposure), constant stress and lack of sleep, drug therapy, injuries of various types. This leads to one or more of the previous eight factors.
As you can see, it all comes down to shifts in the immune system, only the paths to this state are different and include a different number of “steps.” This suggests a fundamental conclusion that eczema does not have a single development scenario. There can be dozens, hundreds of such scenarios. And some experts believe that there are as many scenarios as there are patients with this diagnosis.
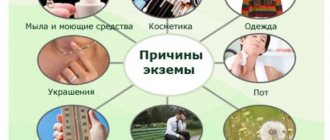
Causes
Despite the prevalence of the disease, the exact origin of eczema has not yet been 100% established.
There is a group of factors that can lead to the development of the disease. They are divided into two subgroups, depending on the source of negative influence.
Endogenous:
- disruption of the functioning of the digestive system (pancreatitis, cholecystitis, gastritis);
- hereditary tendency to develop atopic diseases;
- psychological disorders (depression, neuroses, strong feelings);
- hormonal pathologies (diabetes mellitus, hyperthyroidism).
Exogenous:
- exposure to aggressive substances on the skin (chemicals, alcohols, dyes);
- environmental effects - hypothermia, ultraviolet irradiation, chapping of the skin;
- systematic irritation and injury;
- presence of allergies.
Doctors identify conditions that can indirectly provoke the development of the disease:
- lack of vitamins and microelements (hypo- and vitamin deficiency);
- lack of fatty acids (omega-3, omega-6);
- helminthic infestations;
- immunity disorders.
Symptoms
Eczema is quite rightly considered one of the hand diseases. Even with dyshidrotic eczema, which affects only the legs and arms, inflammation affects the legs in only 20% of all cases. Symptoms on the hands with the described pathology have many common points, but there are also unique manifestations.
The main symptomatic feature common to all species is polymorphism. When symptoms of different stages of disease development are observed simultaneously. With dermatitis, the opposite is recorded - strict, step-by-step dynamics.
True (idiopathic) eczema
Pronounced erythema of irregular shape, the size of red spots varies from a few millimeters to several centimeters. Numerous microvesicles are immature serous vesicles up to 1 mm in diameter. Almost immediately they turn into microulcers (the so-called “serous wells”), from which exudate protrudes onto the epidermis, forming a brownish crust.
After the scabs fall off, a healthy layer remains. But with frequent relapses, hyper- and hypopigmentation of the skin under the scabs occurs, its lichenification - the skin pattern changes, the skin furrows become deeper, and abnormal plateau-type thickenings are noted, reminiscent of flat calluses with deep cracks. Another sign of chronicity is constant peeling, both erythema and scabs. And all this against the background of itching and burning that never completely subsides.
Dyshidrotic eczema
It stands out because it always affects only the hands and feet, with the hands in 8 cases out of 10. At least, the disease begins with the palms. Erythema is mild; usually, the process begins with simple redness of the skin area. Then numerous, rather large (up to 5 mm), serous vesicles appear, sometimes merging into entire blisters. After resolution, weeping ulcers are left, covered with grayish-yellowish crusts. With frequent relapses against the background of dyshidrosis, true eczema often occurs.
Tilotic (horny, callus-like) eczema
The localization is completely identical to dyshidrosis. Erythema and rashes are not expressed due to the rapid formation of callosal thickenings.
Microbial (bacterial, viral) eczema
On healthy, intact skin it occurs only as:
- a spontaneously passing symptom of some kind of infection, for example, a rash with scarlet fever, yersiniosis;
- individual allergic reaction to pathogenic and conditionally pathogenic microflora.
In other cases, this form develops against the background of another skin lesion, when some kind of secondary infection is introduced into the damaged, inflamed areas.
Bacterial eczematous lesions reveal themselves by the presence of many small, pinpoint screenings around the main area and the presence of purulent exudate.
Mycotic eczema
In fact, it is an unusual, additional symptom of a fungal disease, due to the fact that the immune response contains not only a standard reaction to the penetration of a foreign antigen, but also an allergic one. For fungal eczema, the main distinguishing feature is a sharp, very clear delineation of the affected area. Mycoses contribute to the transition of skin pathology into a chronic form, and hormonal treatment, common for eczema, is inhibited by the fact that fungi rapidly grow and mutate under the influence of hormones.
Allergic eczema
Occupational eczema is a special case of allergic eczematous lesion. Inflammation is caused by irritating factors and is of a chemical nature. The irritant can be anything: paint, metal, cleaning product, cosmetic, food, medicine, etc.
Childhood eczema
Differs in weak differentiation. Often there is a complex of not only skin, but also other allergic, infectious and inflammatory processes occurring at the level of the whole organism (bronchial asthma, conjunctivitis, gastrointestinal irritation, etc.). Not so long ago, for children under 5 years old, it was customary to call eczema an exudative diathesis, but later it turned out that such a diathesis is something of a universal “near-pathological” state of the child’s immune system. And against this background, more specific pathologies develop. Although a child’s hands are also attacked at the beginning of the disease, in childhood the process almost always tends to complete generalization at the level of the whole organism. This is why infants are at risk of toxic-allergic shock.
Non-hormonal agents
These can be either antibiotic-containing ointments or ointments with components that accelerate healing, normalize metabolic processes in the skin, and also have an antimicrobial and antiseptic effect.
- Zinc-based ointments help to cope with the signs of weeping of the affected areas and prevent infection. Inexpensive and effective zinc ointment has long been successfully used in dermatology.
- Skin Cap. Has antifungal and antibacterial effects. Can be used in the initial form of relapse of the disease.
- Bepanten, Panthenol, Dexapanthenol. Helps normalize the process of epithelization of ulcers and has a strong regenerating effect. Panthenol-based ointments are safe, do not cause an allergic reaction, and are the treatment of choice for treating skin problems in infants. Timely use of such medicine will help prevent the development of complications.
- Radevit. Contains a complex of vitamins A and E, which normalize the natural regeneration of skin cells and help restore local immunity. In addition, the product effectively reduces itching and swelling of the skin and has a calming effect on irritated epidermis.
- Magnispor. The product is based on medical grease, an oil refinery product that is used in medicine as an antiseptic with a drying effect. When applied to the skin, a special protective film is created that protects wounds from the penetration of pathogenic microorganisms.
- Aurobin . It is used in the initial stages of the disease, when the symptoms are mild. Helps fight skin cracks and heal superficial ulcers. The product can be used to relieve symptoms over a long period of time.
- Also, for the treatment of mild and initial forms of eczema on the hands, the following products are used: Dermasan, Desitin, Eplan, boric ointment .
- Processes accompanied by copious discharge of pus from the lesion require the application of agents containing antibiotics; for such cases, Levomekol ointment is prescribed.
- Ichthyol ointment and balsamic liniment according to Vishnevsky can also be used under a bandage when microbial flora is attached, and if the rash is accompanied by detachment of the outer layers of the skin.
Non-hormonal ointments for eczema on the hands are effective in the initial stages of the disease; if prescribed by a doctor, they can be used in parallel with hormonal treatment, and can also be used to prevent exacerbation of the disease. Many of them can be used during pregnancy.
Photo of eczema on hands: what it looks like
In the first photo you can observe characteristic peeling and lichenification with long-term dyshidrosis.
Content may be difficult to view
The second photo shows redness and pigmentation characteristic of true eczema.
Content may be difficult to view
Main article: What eczema looks like
Anti-eczema medications
Hormonal drugs
Hormonal drugs - act in the deep layers of the epidermis and reduce the process of inflammation in a short time.
Advantages of hormonal drugs:
- achieving quick therapeutic results;
- have general medicinal properties;
- used for all types of eczema;
- allow you to achieve results when regular creams do not work.
Flaws:
- the product is not suitable for all patients;
- creams are not suitable for long-term treatment;
- the remedy must be prescribed by a specialist.
The following types of eczema are most often treated with hormonal medications:
- true;
- seborrheic;
- professional;
- seborrheic;
- periwound;
- microbial;
- dyshidrotic.
If any complications of eczema of various types occur, the use of hormonal agents is recommended.
Non-hormonal drugs
Non-hormonal drugs are intended to block the disease . Most often, such drugs are prescribed for a disease that has decreased in intensity and is not progressing.
Advantages:
- are used for a long time.
- restore damaged skin.
- moisturize the skin.
Flaws:
- effective in complex cases of the disease;
- A doctor's prescription is required.
Non-hormonal agents are used for all types of eczema, but before starting therapy you should find out which cream to choose.
The YouTube ID of Insert video URL or ID here is invalid.
Diagnostics
A dermatologist (sometimes an immunologist-allergist), having studied the patient’s history, his complaints and existing symptoms, almost always makes a correct preliminary diagnosis. This is especially true for those types of eczema that affect strictly defined areas. It is very difficult to confuse it with another disease, for example, dyshidrosis.
In-depth diagnosis is necessary when the symptomatic picture is blurred, or the treatment regimen needs to be clarified:
- general blood test - changes in the leukocyte formula confirm or refute the primary diagnosis: with dermatitis, strong eosinophilia is always observed, and with eczema, eosinophils may be normal, leukocytes are increased, ESR is increased;
- blood test for immunoglobulins - as already mentioned, with eczema there is a high concentration of Ig E and, possibly, Ig G, and Ig M is reduced;
- allergy tests (skin, systemic) - if the root of the problem is an allergic reaction, you can try to identify the main irritant and completely eliminate it from the patient’s life;
- analysis for parasites using the Ifa method (giardia, opisthorchid, roundworm);
- a coprogram showing both the quality of food digestion and the presence of intestinal helminths;
- skin scrapings to determine secondary infection.
A full set of diagnostic procedures sometimes includes examination of the gastrointestinal tract for chronic foci of inflammation.
Types and symptoms
Depending on the type of disease, the symptoms of the rash may differ. The location of the source of the inflammatory process is also of great importance.
Eczema true
The disease can be acute or chronic. It manifests itself as an inflammatory process, which quickly moves into the second stage, the appearance of skin rashes.
Symptoms:
- itching;
- redness;
- appearance of watery pimples:
- crust formation;
- peeling of the skin.
Appears in the area of the hands and feet.
Mycotic eczema
Most often this type of disease occurs as a result of infection with pathogenic fungi.
In order to eliminate the disease, it is necessary to carry out treatment in two stages: the elimination of pathogenic microorganisms and the skin defect.
Has the following characteristics:
- the appearance of round spots;
- peeling of the skin.
It forms on the lower extremities, however, it can also appear in other parts of the body.
Eczema microbial
It appears as a result of infection in skin lesions.
Most often, this type of eczema is acute and manifests itself with the following symptoms:
- round spots with clear boundaries;
- the appearance of a crust on the spots.
It appears on the inside of the hands, shins and in the head area. The disease is accompanied by itching and swelling of the skin.
Treatment of eczema on hands
Therapy is always comprehensive, consisting of:
- antiallergic drugs;
- anti-inflammatory drugs;
- antibacterial drugs;
- painkillers and antipyretics;
- softening and restorative agents;
- non-drug therapy: physiotherapy, sanatorium treatment, preventive measures.
Read more about the above.
Physiotherapy
Almost all physiotherapy involves exposure of the affected tissue to electromagnetic radiation that differs in its parameters:
- Electrosleep is putting the patient into sleep or into a state bordering on sleep for 40 minutes or more using weak currents acting directly on areas of the head through electrodes. The method is especially useful if the etiology of eczema is psychoneurological (at the initial stage of the disease, electrosleep can completely stop its further development).
- Franklinization is nothing more than an “electrostatic shower”, when a low-power direct current is passed through the patient’s entire body. The mechanism of therapeutic effect is similar to electrosleep, but it is better not to undergo this procedure for children under 13 years of age.
- Darsonvalization and other similar methods - high-frequency electrical impulses dilate the vessels of the dermis, improve its trophism and, according to unconfirmed data, enhance the production of the body's own steroids, which have a powerful anti-inflammatory effect.
- Electrophoresis is the introduction of small portions of drugs through the epidermis directly into the dermis using an electromagnetic field.
- Ultraviolet irradiation is a powerful non-drug agent that destroys pathogenic microflora.
- Cryotherapy is the treatment of small affected areas with liquid nitrogen. This causes the inflamed tissue to die, leaving behind fresh, healthy skin.
Despite criticism of physiotherapy in Western medicine, practice shows its positive effect on many skin pathologies, including eczema. The only contraindications are cancer, age under 3 years, and the presence of a pacemaker.
Ointments
All ointments, gels and creams are the main component of topical treatment for eczema.
Actions of ointments:
- anti-inflammatory and partially antiallergic - non-hormonal (Aurobin, Biopin, Dermaref, Magnipsor, Eplan, etc.) and hormonal (Akriderm, Hydrocortisone ointment, Elokom, Advantan, Sinaflan, Lokoid, Afloderm, etc.);
- antibacterial - antibiotic-based ointments (Erythromycin, Gentamicin, Levomycetin, Tetracycline, Zinerit, Dalatsin, etc.), necessary for secondary infections;
- analgesic - any external agents that include menthol, lidocaine and other analgesics, but are rarely used for skin lesions, since itching and burning subside on their own when inflammation and the source of infection are eliminated;
- protective (moisturizing, protective film and nutrition), mainly these are creams - Librederm Seychelles with sandalwood and coconut oil, Avanta Beloruchka nourishing with vitamin E and almond oil, Boro plus intensive care, Topicrem ultra-moisturizing, etc.
It is worth mentioning separately the rather effective means of Soviet medicine: Fukortsin, brilliant green solution, zinc paste. The main effect of these old remedies is to create a protective film over the inflamed area.
Main article: Ointments and creams for eczema
Droppers and injections
In severe cases, tablets are preceded by droppers and intramuscular injections aimed at desensitizing the body:
- droppers with 10% calcium chloride solution, especially effective in combination with 10% sodium bromide solution;
- droppers with 10-20% sodium hyposulfite solution;
- intramuscular injections of 5% ascorbic acid;
- similar injections of hydrocortisone with 0.25% novocaine solution;
- in case of severe general intoxication: intravenously 40% hexamethylenetetramine solution or 10% sodium salicylate solution.
Of course, when such measures are required, the patient is recommended to undergo at least short-term hospitalization.
Pills
Tablets are represented mainly by antihistamines of different classes. But their principle of action is similar - competitive binding to histamine receptors and (for the newest drugs) inhibition of the synthesis of histamine itself. Examples: Suprastin, Loratadine, Desloratadine (Erius), Tavegil, Diazolin, Fenistil, Rupafin (Abbott), Xizal, Zirtec, Cetrin, Kestin (Nycomed). In case of severe intoxication, it is occasionally necessary to bring down the fever with the help of NSAIDs - Analgin, Ibuprofen, Paracetamol.
Main article: Eczema tablets
Diet
A number of foods are undesirable for eczema. Different foods have different degrees of allergenicity.
High degree:
- cow's milk;
- chicken meat and eggs;
- Fish and seafood;
- spicy, smoked, highly salted;
- most berries (raspberries, strawberries, blackberries, blueberries, black currants);
- citrus;
- persimmon;
- melons;
- honey;
- nuts;
- coffee;
- tomatoes, carrots;
- mustard, red and black pepper;
- mushrooms;
- wheat and rye.
Average degree:
- cocoa;
- beef, pork, turkey, rabbit;
- legumes;
- potato;
- peaches and apricots;
- bananas;
- Red Ribes;
- corn;
- buckwheat and oats;
- barley;
- butter and most cheeses;
- fatty cottage cheese.
Low degree:
- venison, horse meat, lamb;
- zucchini, squash;
- plums;
- watermelons;
- white currants and white cherries;
- cucumbers;
- Green pepper;
- spinach;
- gooseberry;
- apples (green and yellow);
- almond;
- blueberry;
- pumpkin and turnip;
- natural teas, especially green tea;
- kefir, low-fat cottage cheese.
If eczema develops against the background of celiac disease (gluten is not digested), then a gluten-free diet is developed separately.
Main article: Diet and nutrition for eczema
Treatment with folk remedies at home
Traditional medicine is excellent as an additional therapy during exacerbation and as a primary therapy during remission. All components of the recipes are sold in the nearest supermarket and pharmacy.
Here are some examples:
- 2 tbsp. add spoons of sea salt to 1 liter of very warm water, put your hands in the bath and hold until the water reaches room temperature, once a day for 2 weeks;
- pour at least 100 grams of oat straw into 1 liter of boiling water, leave for 2 hours, strain, soaked straw is used to apply bandage compresses to sore skin (keep the compress for at least 90 minutes), the frequency and duration of the course is based on symptoms;
- Mix 200 grams of any vegetable oil with laundry soap, rosin, aloe juice and beeswax (take 50 grams of each). Melt all the ingredients over low heat until a homogeneous mixture, which after cooling should be applied to the inflamed areas 2 times a day for at least 10 days;
- freshly squeezed parsley juice helps a lot when rubbed regularly (2 times a day), an analogue is a compress of freshly grated parsley;
- if you pick a willow twig, resin will soon flow from it - an excellent natural ointment for eczematous skin, it is more convenient to apply with a thin wooden stick, once a day for at least 2 weeks.
But the attending physician must be aware of all the methods used.
Main article: Treatment of eczema with folk remedies
Recommendations
For any eczema, at least in the acute stage, it is strongly recommended to follow some rules aimed at protecting the dermis:
- do not use aggressive cleaning agents (especially without gloves and a mask);
- detergents and cosmetics should all be hypoallergenic and emollient;
- do not allow skin contact with very cold or too hot water;
- Avoid prolonged exposure to direct sunlight on unprotected skin;
- if necessary, follow an antiallergic diet;
- in clothing and underwear, the skin should not come into direct contact with synthetics or wool.
The patient himself gradually determines what should be avoided so as not to aggravate the condition.
Main article: Treatment of eczema
Akriderm and its three varieties
The main active ingredient of the ointment is the corticosteroid betamethasone, it is a highly active hormone and is 25 times stronger than hydrocortisone.
The ointment helps relieve itching in severe forms of eczema and other dermatoses accompanied by severe inflammation, skin damage and tissue swelling: chronic urticaria, psoriasis.
For complicated forms of eczema, there are also varieties of the drug, supplemented with active pharmacological components; such an ointment can be recognized by the presence of additional letters in the name:
- Akriderm GK contains a broad-spectrum antibiotic, gentamicin, and an antimycotic drug, clotrimazole. Suitable for the treatment of mixed fungal-microbial dermatitis;
- Akriderm S contains salicylic acid, which helps fight hyperkeratosis in eczema and accelerates the cleansing of dead cells in cases of severe peeling in the area;
- Akriderm Genta with gentamicin solves the problem of eczematous ulcers infected with microbes.
It is strictly contraindicated to use types of ointments with auxiliary medicinal substances without special need and symptoms of concomitant complications.
Also, the active ingredient of the drug (betamethasone) is the basis for other external remedies for eczema: Belogent (for microbial form), Triderm, Betliben (for the treatment of eczema due to allergies).
Prevention
It is recommended to adjust your lifestyle:
- during remissions, protect the skin with protective creams and balms (especially in winter);
- normalization of personal hygiene;
- nutrition should be balanced and as natural as possible;
- stress should be kept to a minimum, healthy and long sleep is regularly necessary;
- moderate outdoor sports activities;
- periodic health resort treatment;
- eliminating or suppressing associated factors (for example, avoiding allergies);
- serious restriction in alcohol consumption, smoking cessation.
And the main thing is not to ignore the beginning inflammation on the skin, but to stop the process immediately
Dyshidrotic
This type of disease most often appears on the extremities and has the appearance of small blisters containing clear liquid and after damage, specific crusts appear that can cause itching and burning sensation.
Most often they are localized on the palms and soles; in rare cases, symptoms are observed on the skin between the fingers.
Tilotic
The disease occurs as a result of prolonged contact with chemicals or regular exposure of the skin to foreign objects, as a result of which the outer layer of the skin thickens and lesions form.
Symptoms:
- formation of skin compactions in the form of calluses;
- the appearance of a large rash with a dense structure;
- the formation of cracks and wounds in places where the epidermis is compacted;
- pain and itching sensation.
This type of disease leads to impaired skin mobility and most often manifests itself in the area of the palms and feet.
Occupational eczema
This type of disease occurs as a result of prolonged contact with irritants such as resin, household chemicals, dyes, nickel, etc.
Symptoms:
- the formation of papules that secrete fluid;
- itching
The defect can occur in the area of the arms, neck, forearm, and lower leg.
Sycosiform
Belong to a microbial type of disease. Occurs most often in people who suffer from sycosis. Manifests itself in the area of hair growth and location of hair follicles.
Symptoms:
inflammation of the follicles;
- formation of red spots at the site of hair growth;
- the affected areas quickly increase in size;
- itching and burning sensation;
- thickening of the stratum corneum of the skin.
The disease most often manifests itself on the face, armpits, and groin area.
Complications and consequences
In general, the disease is not fatal for an adult. Rather, it is exhausting and causes a lot of discomfort.
Rarely, more serious events are possible:
- allergic shock with increased sensitization of the body;
- transition of a secondary skin infection to the systemic level, development of general sepsis;
- inflammation leads to accelerated synthesis of new cells, and this always increases the risk of cells with disrupted DNA structure - cancer cells.
There is a direct relationship between the intensity and frequency of exacerbations and the risk of complications.
Home treatment and diet
It all depends on what side effects and complications the eczema caused. To speed up recovery, patients are prescribed physical therapy, which helps relieve inflammation of the skin. For the entire period of treatment it is worth switching to dietary nutrition.
You must stop using:
- spicy and salty foods;
- eggs;
- fried meat;
- smoked products;
- meat broths;
- alcoholic and alcoholic beverages;
- cheeses;
- coffee;
- chocolate;
- conservation.
You can treat eczema on your hands at home, but use various folk remedies only on the recommendation of a doctor. In any case, a person carries out the main therapeutic course at home, taking pills and other medications according to a schedule.
Features in children
In childhood, the main set of symptoms is the same as in adults. But childhood eczema is very “greasy”. Moreover, it poses a serious threat to a small child. The baby’s body may simply not withstand intoxication. Therefore, childhood eczema requires special urgency and at the same time caution in treatment. After all, there is another problem - the younger the child, the narrower the range of medications acceptable for use.
Main article: Eczema in children
Rules for prescribing local treatment
- when symptoms are of low intensity, it is recommended to use non-hormonal creams;
for eczema, which is accompanied by a high level of dry skin, it is necessary to use oil-based ointments;
- after using hormonal drugs at the last stage of recovery, creams with a light texture are prescribed;
- in case of a sharp complication of the disease, complex treatment in the form of ointments and hormonal drugs can be prescribed.
The choice of any of the medications requires the prescription of the attending physician.
The occurrence of eczema requires the appointment of correct therapy, otherwise complications may develop that will gradually become chronic. To obtain visible results, it is recommended to observe regular treatment and proper care of damaged skin.
During pregnancy
The difference from the general scenario here is that the treatment of eczema during pregnancy is complicated by the inadmissibility of the mother taking most medications. Whatever drug you take, everywhere in the instructions, the “Contraindications” column contains the inscription “pregnancy and breastfeeding.” The most vulnerable period is the 1st trimester. Although, in especially severe cases, under the supervision of a doctor, a pregnant woman is prescribed all the necessary medications. By the way, eczema can even be triggered by hormonal changes in the body during pregnancy. Such eczema, as a rule, gradually goes away on its own after childbirth.
Childhood eczema
This type of disease most often manifests itself at an early age during artificial feeding, since the immune system is not able to independently cope with various viral infections.
Eczema initially manifests itself with mild symptoms, which gradually increase and include signs of seborrheic, microbial and true eczema.
Symptoms:
- pink small formations that quickly become damaged and form a crust;
- elevated temperature;
- the skin around the formation swells and takes on a red tint.
Most often, this type of disease begins to appear in the area of the child’s cheeks and forehead. Most often, children aged 3 months and older are exposed to this type of disease.