Sometimes hearing the diagnosis of a warty nevus in an adult or child causes a panic reaction. But it is worth noting that a growth of this type is a common birthmark or an ordinary mole (a massive accumulation of cells with a large amount of pigment). And the additional word “warty” explains that the mole has the shape of a wart.
Epidermal warty nevus causes and features.
Epidermal verrucous nevus is a cutaneous hamartoma-type tumor consisting of keratinized tubercles that often aggregate into plaques with various clinical manifestations. The fact that it belongs to hamartomas means that during the process of embryonic development, due to some reason, a mistake was made. And now the fabrics don’t look as they should. In a warty nevus, there is a violation only of the number of normal structures of the epidermis without any atypical cells - this is the main reason. It is also called keratinocytic epidermal nevus. This type of nevus should not be confused with papillomatous nevus, which has a completely different structure. Occurs in one in 1000 people. Mostly detected at birth. But, sometimes, it can be discovered later when noticeable hyperkeratosis develops, resulting in a warty surface and dark coloration. Verrucous nevus increases proportionally as the child grows, but some tend to minimally expand into adjacent areas of skin in later life. A mole exists throughout life and usually does not cause subjective complaints or concern. In most cases, this single formation, sometimes, can be associated with various abnormalities, being a sign of epidermal nevus syndrome. A verrucous nevus increases the risk of secondary skin malignancies, that is, it can cause skin cancer.
What do experts advise?
Do not forget that aggressive growth of verrucous nevi can be malignant. This suggests that it is necessary to avoid any heating of the skin growths. Based on this, experts advise:
- refuse to visit baths and saunas;
- in hot weather, do not stay outside for a long time (from 11.00 to 16.00 - it is during this period of time that the exposure to ultraviolet radiation is greatest);
- protect yourself as much as possible from direct ultraviolet rays coming into contact with the affected skin;
- it has been proven that sun creams do not in any way provide protection against the appearance of cancer;
- Refusing to use a solarium to get a tan is harmful.
If you notice that the growths have changed their shape or have acquired a new shade, then you should immediately consult a doctor. With timely preventive treatment, the nevus will not be malignant, and its neutralization using modern methods will allow you to get rid of discomfort.
One important rule to remember is that self-medication can be dangerous to your health.
Removing the tumor using any home method can provoke inflammatory processes or severe irritation of the epidermal layer. Moreover, the latter action will also help accelerate the progression of cancer cells, if they are hidden in the body. Be sure to monitor your immune system - only it will save you from the manifestation of the harmful disease HPV. The article has been verified by the editors
Warty nevus: varieties and photos.
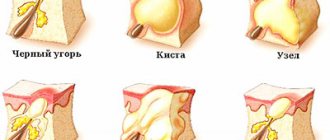
Clinical varieties of epidermal verrucous nevus have been described due to the distribution pattern, prevalence, and existence of an inflammatory component.
Verrucous verrucous nevus.
Verrucous nevus, in the insular form, is located in a single region of the body, and the size of the formation is relatively small. In appearance, the typical manifestations of this subtype of nevus are yellowish-brown or dark brown warty plaques, consisting of grouped flat-topped or papillomatous tubercles. There is no or minimal redness and inflammation. Some moles are soft and have a velvety surface. Multiple smaller bumps often form around large growths (see photo). Similar in appearance skin diseases are seborrheic keratosis and papillomatous melanocytic nevus.
Unilateral linear warty nevus.
An epidermal nevus with unilateral spread and involvement of large areas is called a linear unilateral verrucous nevus. More common on the trunk and limbs. This variety is presented as linear streaks on the limbs or as tufts on the body due to its distribution along Blaschko lines, as in the photo below. However, these lines are not always as long as Blaschko lines. Usually, only some areas within these lines are affected, alternating with intervals of healthy skin. Sometimes a warty nevus of this variety affects half the body, moving from the scalp to the face, neck towards the back, shoulder, hand and leg. All parts of the body are involved without crossing the midline anteriorly or posteriorly, thus showing a line of strict separation from the healthy half of the body. In children, this linear warty nevus may be flat and light colored, but in later childhood it often becomes raised and darker in color. Tumors in the area of the hands and feet are usually more keratinized. The surface of warty nevi is hairless. However, there is a separate rare variant of linear verrucous nevus, covered with white, thin and long hair.
The photo shows a warty nevus of the most common linear shape. Lighter and less convex options are possible.
A unilateral warty nevus on the face near the eye involves several Blaschko lines at once.
Generalized warty nevus (spine ichthyosis).
Generalized warty nevus covers wide areas of the trunk, limbs and head on both sides. Skin lesions are located along Blaschko's lines. In the majority, they have a symmetrical distribution on both sides of the body of varying lengths, typically stopping exactly in the middle. Some growths merge. This type of verrucous nevus is one of the most extensive on the skin and causes serious cosmetic and problems.
Inflamed linear epidermal warty nevus.
This is a linear epidermal verrucous nevus with an inflammatory component. This tumor subtype is typically unilateral. In most cases, it occurs on the limbs and in the lower half of the body, especially on the buttocks. It is more red, scaly and itchy than a classic warty nevus. Thus, it may be mistaken for lichen linearis, psoriasis vulgaris, or lichen planus. Although, these inflammatory dermatoses are mostly acquired. Sometimes, differences in these diseases are confirmed only by histological examination.
Inflamed verrucous nevus is similar to many other skin conditions. More often than other options it turns into skin cancer.
A generalized warty nevus completely covers the skin of the upper half of the body. The tendency to form lines remains.
Kinds
Depending on the prevalence of age spots, verrucous nevi are called systemic or localized.
Systemic verrucous nevus stretches along the body and visually looks like a “garland”. You can recognize it by the following signs:
- The systemic formation includes a number of convex birthmarks of an elongated shape, which are characterized by a large extent.
- Every part of the body can become a capture area. Basically, such “decorations” appear along large blood vessels.
- The top layer is characterized by heterogeneous pigmentation, mainly black-brown.
- The surface is granular, hard to the touch, wrinkles and cracks are clearly visible.
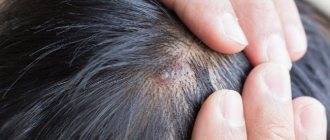
Localized verrucous nevus is based on a limited area of the body and can affect the scalp. “Wart” has characteristic features:
- A single arrangement or several formations tightly pressed against each other are possible.
- The surface is rough, strewn with small cracks, and very rarely has hair. This birthmark may look like a cauliflower inflorescence.
- The size of the mole is small - about 1 cm on average.
- The characteristic color is close to dark brown; there are also nevi in the shade of normal skin.
Warty nevus, diagnosis.
Large unilateral or generalized warty nevi are diagnosed clinically, by appearance and manifestations. Generalized keratinizing lesions of a similar pattern with a generalized verrucous nevus are sometimes observed in the early stages of some genetic diseases. Histological characteristics of a warty nevus, such as acanthosis, hyperkeratosis, papillomatosis, are not specific and are common in all clinical varieties. There may be striking similarities with seborrheic keratosis, acanthosis nigricans, and Hopf's acrokeratosis verrucous. The relationship between the clinical picture and histology gives us a diagnosis.
Prevention
The use of medications to prevent the disease is important for a child under 2 years of age (if there is a family member who suffers from this disease) and in case of problematic localization of the growth (contact with clothing, etc.). For preventive purposes, dermatologists advise using ointments or creams containing vitamins A, E and salicylic acid.
Since there are cases of the development of tumor diseases due to warty growths, you should remember the basic rules for protecting against such consequences. Doctors advise forgetting about visiting a solarium or bathhouse. In summer, when the outside temperatures are high and the sun is scorching, it is better to avoid prolonged exposure to direct sunlight.
How dangerous is a warty nevus?
Verrucous nevus is a precancerous lesion that can potentially develop into squamous cell skin cancer if left untreated. Constantly inflamed, injured, tanned formations are more susceptible to developing into cancer. Various infections can develop within the verrucous nevus, such as bacterial eczema and pustular infections, and they may spread from here to neighboring areas. First of all, scratches in the area of the nevus contribute to this. If located in areas subject to friction, such as the groin and axillary areas, which become softer, warty nevi become more easily a source of infection. Lesions on diaper rash surfaces acquire an unpleasant odor due to infection. Positioning in visible areas is embarrassing and distressing to the patient. Common warty nevi can cover most of the body. Moles located on the hands and feet cause destruction of the nails.
Local and medicinal treatment of warty nevus.
- Patients and doctors should remember that topical application of various ointments can only improve the appearance by removing the upper layers of the epidermis. However, the warty nevus and all its manifestations return again as soon as the use of ointments is stopped. However, greater destruction of the epidermis is necessary, which can only be achieved by medical methods.
- Topical application of corticosteroids, which can be in the form of ointments or injections, may provide some mild relief by reducing inflammation and itching.
- Isotretinoin ointment (retinoic ointment) may also partially help. This modified vitamin A can improve the differentiation of epithelial cells of the warty nevus, reducing negative manifestations.
- Calcipotriol cream may reduce dryness, but should be used with caution due to possible side effects. Salicylic acid may have a similar effect. Podophyllin and 5-fluorouracil are also effective, suppressing cell proliferation in the upper layers of the epidermis. In some cases, this may lead to partial removal of the verrucous nevus.
- The use of modified vitamin A (Roaccutane) tablets is useful for the treatment of common warty nevi, but requires lifelong use.
Forecast
The prognosis is favorable. Verrucous nevus usually does not grow and does not transform into cutaneous melanoma. However, the situation may change if the nevus is permanently injured. Chronic injury can give rise to the growth of a nevus and cause it to become infected.
Nevus Ota
Previous
Borderline skin nevus
Next
Warty nevus, removal in the clinic.
- If the warty nevus is small, they try to remove it in various ways in the clinic. With incomplete superficial removal, relapse is possible. If overzealous, rough scars are possible. For these purposes, surgical treatment, cryodestruction, electrocoagulation, dermabrasion, laser and radio wave removal are used.
- Surgical removal will always be accompanied by the appearance of scars. This is how the skin is removed to its full depth using this method. Other methods can only remove the upper layers of the epidermis, and deeper layers are not required. However, there is still the possibility of a relapse occurring months and years later.
- Dermabrasion is too superficial a method, brings only temporary relief, and is associated with a very high probability of relapse. If dermabrasion is too deep, thick scars are possible.
- Cryodestruction is accompanied by swelling, delayed healing, and white or dark spots are possible after the procedure. However, for small warty nevi, cryodestruction is a good alternative.
- It is most preferable to remove a warty nevus with a laser. Modern devices allow you to control the depth of removal. Small growths are evaporated by laser in one session. Large skin lesions will require multiple sessions.
- It is also possible to remove a warty nevus using the radio wave method and an electrocoagulator, however, the depth and accuracy are much more difficult to control than with a laser.
Therapy with folk remedies
Not every person can afford treatment in a specialized clinic, which is why many choose treatment with folk remedies. Celandine juice helps to cope well with the disease. It must be applied to the mole and secured with a band-aid. This procedure is carried out until the tumor completely disappears.
You can successively apply garlic and then lemon juice to the mole. The duration of the procedure is 7 days. A tincture of apple cider vinegar and garlic helps to cope with the disease. Before using traditional methods, you should definitely consult with your doctor regarding their safety.