Moles (aka nevi) are benign formations that may not cause problems to a person throughout his life, but can cause a serious condition, turning into a malignant tumor - melanoma . One of the signs that trouble is occurring with a mole is roughness, flaking of the formation and its dryness. It is possible that these changes will not lead to cancer, and the reasons for such changes are quite harmless, but it is advisable to have this confirmed by a dermatologist.
Dermatological diseases and peeling moles
A very large group of reasons for peeling skin over moles.
The most common:
- allergic processes;
- genetic – ichthyosis;
- psoriasis;
- pityriasis versicolor;
- seborrhea;
- contact dermatitis.
The list can be continued for a very long time.
It is important to remember one thing: if dermatological pathology manifests itself as peeling and affects areas of the skin with moles, then this is a reason to consult a dermatologist and undergo a course of treatment.
Problems usually arise among those who do not want to be examined by a specialist and try to cure themselves.
Allergies
are a very common cause in modern civilization.
Character traits:
- the skin turns red;
- small urticaria-type rashes or large, dense papules appear;
- the involved areas itch, itch unbearably;
- As the allergy resolves, fairly large areas of peeling may remain at the site of the rash, including moles.
The beginning of the process after contact with an allergen (which one is an individual matter) indicates in favor of an allergic component.
Ichthyosis
This genetic pathology is not that uncommon.
There are cases in dermatological practice when large areas of the dermis of children peel off along with the moles located on them.
External signs depend on the severity of the disease: from dry skin to deep cracks.
Psoriasis
Another common reason for peeling.
Moreover, such a process is a characteristic sign of this disease.
The scales peel off almost like flakes.
But since only the epithelium of the stratum corneum (which is continuously renewed) disappears, the moles located deeper (nevi) do not disappear anywhere.
True, they can hide under plaques and become invisible.
Pityriasis versicolor
This is a fungal disease, the sign of which is a limited area of peeling, as if consisting of several spots.
The shape is round, the edges are uneven, scalloped.
The formation is painless, but in some people it itches.
Naturally, the focus of pityriasis versicolor can occur above the mole.
If it is also small in size, then sometimes it seems as if a mole is peeling off.
Although this is not true.
Seborrhea
A common phenomenon is when sebum synthesis is too active.
Quite often such problems arise on the head.
Foci of different sizes are formed, covered with loose yellowish scales, which literally peel off in layers.
Seborrhea occurs in children and adults.
The affected surface shines and peels, which is why it becomes a frequent reason for contacting dermatologists.
Contact dermatitis
Most often, these will be local allergic reactions in response to contact with allergenic fabric, detergent residue, grass, and so on.
They differ in that itching, redness and peeling occur to a limited extent.
Only on the surface of the body that came into contact with the allergen.
Why does a mole dry out?
There are several safe reasons why a nevus can change shape, dry out and disappear altogether. Often, neoplasms on the body have nothing to do with the production of melanin. These are so-called papillomas that appear on the human body due to infection in the blood. Papillomas can appear on their own and then disappear. Sometimes these neoplasms are quite difficult to distinguish from ordinary moles. Only a qualified specialist can do this.
Hormonal changes are another reason for the development and death of nevi. A large number of moles on the human body appear during puberty. New growths begin to actively dry out and peel off during the period of decline of reproductive function in women and men. Representatives of the fairer sex often complain that the nevus dries out and begins to itch during menopause. If a mole changes during the childbearing period, it is worth making an appointment with an endocrinologist.
Frequent mechanical damage to moles can lead to inflammation. In this case, the neoplasm will also peel and itch. If the new growths itch and cause considerable discomfort, it is possible that they are affected by a fungus. If the nevus was damaged, but infection was avoided, there will be no pain. A crust on a mole in this case is a good sign. If the nevus is often injured, it is recommended to remove it surgically.
Excessive tanning can lead to malignant degeneration of nevus
Problems with a mole
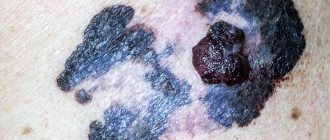
The greatest danger that nevi pose is the risk of degeneration of benign pigmented neoplasms into an aggressive tumor of melanocytes - melanoma.
This cancer accounts for only 4% of all skin tumors.
However, the particular aggressiveness and tendency to metastasize make melanoma a very dangerous process.
The high incidence of skin cancer is not associated with melanocytes, but descavamation is very characteristic of them.
When to go to the doctor
Dryness, roughness and flaking of a mole are signals that you need to visit a doctor, regardless of the reason that caused this condition. The specialist will conduct an examination and determine whether there are objective indications for removing such a formation.
Indications for mole removal
- actual roughness , increased dryness and peeling of the nevus;
- non-compliance of the surface of the mole with the standards of benign formation - correct shape, softness, smoothness, absence of compactions;
- the presence of bleeding or discharge of pus from the growth;
- thickening of the mole itself and the skin around it;
- pain when touching the formation;
- change in the color of the nevus, its shape and size (if it has increased to 6 mm and continues to grow).
It is important! If the dryness and roughness of a nevus is accompanied by at least one of the symptoms listed above, a specialist will most likely prescribe its removal, since only this measure will help to promptly eliminate the source of malignancy and prevent the development of skin cancer - melanoma.
Non-melanocytic processes during desquamation
Their source is the cells of any of the layers of the dermis or epidermis.
Let's look at the most common causes of cancer processes that are not directly related to moles.
Seborrheic keratosis, seborrheic wart or keratoma.
It starts with a small spot covered with yellowish scales.
It grows gradually and after a few decades reaches 6 cm in diameter.
Because of its coloring and loose scales, seborrheic keratoma is sometimes mistaken for a mole that has begun to grow and peel off.
The mole itches and flakes: causes and likelihood of degeneration into melanoma
A mole peels off - this is a situation that forces you to pay attention to the nevus. In its normal state it does not cause harm, but sometimes it reminds of its presence on the body. The tumor begins to peel off, itch, enlarge, and change color. The symptoms should not be ignored; they appeared for a reason. When they appear, there is a danger of degeneration into melanoma.
Is peeling a mole dangerous?
Pigment spots can be congenital or acquired. Congenital ones are harmless. If moles itch and peel, degeneration begins and serves as a reason to remove the stain.
There are up to 30 spots of varying sizes on the body, which is considered normal. The formations differ in melanin content, the pigment gives an individual color. It can be red, beige, bluish, and sometimes the area becomes flat and black.
Acquired spots appear during hormonal imbalance, due to genetic predisposition, from prolonged exposure to the sun. Sometimes moles flake but do not itch. They are reborn and appear in other places.
If symptoms occur, you should consult a specialist.
Causes of peeling
According to doctors, every nevus present on the body, under the influence of certain factors, can transform into melanoma. Melanoma is a malignant tumor. If its appearance changes, attention should be paid to the nevus; it may degenerate into a malignant tumor. People with fair skin are mostly affected by the problem.
External factors
- Sun. The head is a dangerous zone for the development of melanomas; the cancer cell begins to actively react to dryness and exposure to the sun. If you are exposed to the rays for a long time, the skin exhibits a protective function and the cover begins to peel off. The reason for the process is the necrosis of the epithelium, which peels off over time and is replaced by a new layer of cells.
- Artificial tan, obtained in a solarium. The tanning time is reduced due to an increase in ultraviolet radiation.
- Chemistry. The skin is exposed to substances that cause irritation. The stain may peel off from a chemical burn. Substances include alcohol, alkali, acids, solvents, paints, acetone and resins. Cosmetics contain such components, peeling begins from use.
- Radiation from X-rays. Peeling begins if several photographs are taken for certain reasons. If the patient is completely healthy, it will not affect the skin condition.
- Mechanical damage. If you are regularly exposed to friction against the surface of clothing or a belt, consider removing the nevus.
Internal factors
- Type of skin. Skin type at birth influences the subsequent outcome of spots. If a person is born with fair skin and blue or green eyes, they are at risk of developing melanoma. It is recommended to contact an oncologist.
- Age. After 50 years, a complex change occurs in the body, the aging process intensifies, and organs are more susceptible to cancer. If peeling continues for several weeks, you should consult a specialist to remove the formation.
- Reduced immunity. Occurs for a variety of reasons and can contribute to changes in education.
- Tobacco smoking. Reduces the body's defenses, which increases the risk of stain degeneration.
- Genetics. When the gene responsible for destroying atypical cells changes, cancer cells multiply, and subsequently the moles flake and flake off.
What to do when peeling and how to stop the process
Diagnostics is the first aid when detecting abnormal changes in formations. Using lasers, dermatology has learned to eliminate the malignant type of moles that begin to become inflamed.
If you find signs of changes in the surface of the nevus, contact your oncologist. It is forbidden to self-medicate or use dubious means to remove peeling.
Pigment spots form during pregnancy. Regularly inspect any stains that appear; the surface should not be scaly. Drying, coarsening, and darkening must be avoided. Choose a fabric that will not irritate your skin.
When to see a doctor and associated symptoms
Contact a specialist if you notice symptoms of nevus transformation into melanoma. A nevus that can peel off is considered dangerous.
Signs of transformation:
- the appearance of bleeding;
- change of size;
- appearance of a halo;
- swelling, pain on the surface;
- hair loss.
Doctors remove convex formations located on the neck and waist, where mechanical stress occurs.
It is forbidden to remove it yourself; it will lead to the formation of cancer cells. It is not recommended to choose treatment or creams to remove itching on your own.
In patients who come in with peeling moles, benign formations are more often discovered after examination and do not pose any danger. Sometimes malignant growths are discovered and removed.
Possible complications and precautions
Peeling of the nevus is not the only unfavorable sign. Experts identify signs of transformation of a nevus into melanoma.
Causes the following complications:
- The appearance of cracks, crusts, and ulcers on the skin that begin to bleed.
- Hair loss.
- Color changes.
- The coloring is uneven.
- Itching, pain.
- A rim appears.
- The sizes are increasing.
- The borders merge with the skin.
If the appearance of the nevus changes, consult a doctor. If the formation is benign, it does not grow, does not undergo transformation. The appearance of the described symptoms is a sign of degeneration into melanoma.
Link to main publication
articles:
(1 5,00 of 5) Loading...
Didn't find suitable advice?
or see all questions...
Source: https://ProMelanin.ru/rodinki/shelushitsya.html
Papillomatosis as a cause of peeling
A very common process, often provoked by human papillomaviruses.
Outwardly it looks like a small outgrowth of skin, single or multiple.
People sometimes call this formation a pedunculated mole, although papillomas are not classified as pigmented formations.
Unfortunately, they can become malignant and transform into squamous cell skin cancer.
The most common malignant cause of peeling is basal cell carcinoma.
This is a relatively rare metastatic tumor.
It grows slowly and often appears on the scalp, face and other exposed parts of the body.
One form, nodular basal cell carcinoma, may contain patches of melanin, which makes it resemble a large, growing mole.
Areas of peeling are observed around the pigment spot, crusts are formed, and the color of the node becomes uneven.
For squamous cell carcinoma, desquamation is not as common.
This process often occurs with lesions at the site of previously benign tumors.
For example, where there was recently a hanging mole.
Separately, it is worth dwelling on hemangiomas.
These are vascular, benign tumors that in the early stages look like a reddish spot and can easily be confused with a mole.
Often found in children.
Typical location:
- on the lip;
- on the skin of the back;
- on the genitals (labia, vulva, foreskin of the penis).
Hemangiomas of the abdomen and extremities are less common.
Peeling is not typical for them.
It may indicate either a near resolution of the process (spontaneous recovery from hemangiomas is not uncommon) or a progression of the pathology.
Treatment methods
photo dermatoscopy of moles
The most popular methods for removing birthmarks and convex moles are the laser method, cryodestruction, electrocoagulation and radio wave method. These methods are used to get rid of elements up to 2 cm in size. Excision with a surgical scalpel is carried out with ambiguous biopsy results and at the discretion of the doctor.
- The laser method is considered the most effective way to get rid of skin tumors. Painful sensations during removal are minimal; local anesthesia can be used by subcutaneous injection of lidocaine. The wound heals quickly - within 2 weeks. Healing takes place under the scab, so it does not have the opportunity to fester. The operation is bloodless.
- The cryodestruction method is inferior in cost to the laser method and does not require such qualified personnel. Liquid nitrogen or dry ice freezes the tissue, which leads to the destruction of the nevus. This method is painful and therefore requires anesthesia. Healing is slower and the likelihood of infection is high.
- Electrocoagulation is a method of using electric current. The operation is bloodless, but quite painful. After removal, a scar remains.
- The radio wave method allows you to get rid of small elements. Removal is almost painless and highly effective. There is no bleeding. This method involves contactless removal of the tumor. The healing process takes 1.5-2 weeks.
Ignoring changes that occur with moles and age spots can have serious consequences. Melanoma is considered the most insidious and malignant tumor, as it metastasizes to internal organs with a tumor thickness of 2 mm. In order to prevent the degeneration of a benign neoplasm, it is necessary to exclude or minimize direct sunlight on moles, maintain proper immune activity and visit a dermatologist 1-2 times a year if there are a large number of moles.
Melanocytic processes during desquamation of a mole
Let us remember that melanoma accounts for only 4% of malignant skin tumors.
However, even this possibility must be taken into account.
Almost all melanomas develop from nevi (moles).
When this happens, five visually detectable parameters of pigment formation change:
- Asymmetry appears.
- The edge is “blurred”.
- The color changes - it lightens or darkens, the nevus can become spotted.
- The diameter increases.
- Changes increase (the focus evolves) over a relatively short period of time, several weeks or days.
At the same time, the degenerating mole itches, hurts, is easily injured, and at times peels off.
However, desquamation is not typical for most melanomas.
Rebirth
There are a number of dangerous reasons that cause changes in the condition of the nevus. It peels off due to transformation into melanoma. In this case, peeling and itching are the cause of the increase in size. Cells begin to degenerate.
The nevus urgently needs to be shown to an oncologist and dermatologist if suddenly, along with the above signs, the following appear:
- bleeding;
- increase in size;
- a halo appeared around the mole;
- the surface is swollen and painful;
- noticeable hair loss.
Under no circumstances should you remove anything yourself - this can cause cancer.
Doctors recommend removing convex formations in areas such as the neck or waist immediately in order to avoid accidental mechanical damage or tearing of the mole. Often in patients who come in with a peeling problem, the symptoms turn out to be harmless to the body and have no reason to panic. But in some cases, peeling can cause the appearance of melanocyte-containing cells and the formation of a malignant tumor.
It is not advisable to use medications on your own to remove itching and peeling. Consultation with a professional specialist in this field is necessary.
Diagnosis of peeling moles
You should always contact a dermatologist when:
- the mole grows rapidly, increasing in size daily or weekly;
- the structure of the nevus changes - it thickens, becomes hard, or vice versa, disintegrates, falls apart;
- peeling above it covers new areas or, on the contrary, becomes concentrated, limited and transformed into crusts;
- a mole was injured with bleeding (even if the bleeding stopped quickly);
- the spot hurts and itches a lot;
- the nevus falls off on its own, as if peeling off;
- and in any other cases when a mole behaves suspiciously or a patch of peeling appears on the body.
Every year or every 6 months, all people who have many moles (more than 50) need to see a dermatologist.
And if they also begin to peel off, then you need to make an appointment immediately.
Diagnosis is quite simple: dermatoscopy.
An experienced dermatologist examines the suspicious area of skin under multiple magnification and good lighting.
And, if he finds signs of infiltrating growth, he suggests removing such a focus.
However, there are indications for removal for ordinary, benign nevi.
When they are potentially dangerous by degenerating into a cancerous tumor.
What to do
Although the reasons that a mole has become rough and hard may be completely harmless factors, the elimination of which will lead to the disappearance of symptoms, the changed formations can still lead to sad consequences if you try to cope with them on your own.
Categorical no
- comb , scratch and pick at the formation , as traumatizing it will increase the likelihood of degeneration into skin cancer;
- smear the mole with iodine and brilliant green for cauterization, since both of these substances have an alcohol base, and it stimulates the dilation of blood vessels in the skin and increased nutrition of the mole cells, which is why it will quickly grow in size;
- pull out or shave the hairs on the mole, which will also damage it and push it to degeneration.
Important
- provide protection for rough and dry formations from sunlight;
- do not allow such formation with chemicals and cosmetics ;
- protect the nevus from all kinds of mechanical damage ;
- if a mole is damaged, use an antiseptic and a bactericidal adhesive plaster , then consult a doctor as soon as possible.
Photo 2. If the mole is convex, it is better to remove it or at least cover it with a band-aid.
Source: Flickr (Zeynep Kübra Sağın). Note! A person with moles that suddenly become dry, rough and hard should regularly visit a dermatologist, even if such a condition was initially caused not by pathological, but by everyday reasons.
Examination of a cracked mole
An oncologist-dermatologist can take a scraping from a damaged nevus or some material for histology. In both cases, the pathologist will determine whether there are cancer cells in the tissues. After the analysis, it will be possible to remove the mole using the method recommended by the doctor.
Today there are several methods:
- surgical;
- laser;
- radio wave;
- a liquid nitrogen;
- electrocoagulation.
The method is chosen by the doctor himself, since everything depends on the type of mole, its size and location.
Sometimes it may be necessary to re-analyze the materials, then the liquid nitrogen removal method is excluded, since nothing remains after it, the tissues are simply burned.
When a mole is removed, the skin becomes covered with a crust, which falls off after a while.
Based on the results of histology, the doctor makes a conclusion about the presence or absence of cancer cells in the removed tissue. If the result is negative, and the nevus is cracked due to some physical impact on it, then you don’t have to worry about anything and lead a normal life.
If the result is positive and cancer cells are found in the nevus, then they can be found in other moles. The doctor must carefully examine the adjacent skin formations and take their particles for testing. In addition, it will be necessary to undergo a complete examination of the body. Based on the results of all procedures and tests, the doctor will give an opinion on what stage of cancer the patient has. There are 4 of them in total. The last stage is practically untreatable, which is why it is so important to identify the disease in the early stages in order to start therapy on time.
If melanoma is suspected, the mole should be preserved and sent for histology
Reasons for appearance
If a mole becomes uneven to the touch, itches and peels, then most likely it was influenced by external factors. One of the most aggressive is the sun's rays. Sunbathers often notice that the mole has dried out and shriveled. Such a change in the tumor occurs after mechanical impact: friction, impact, burn with a chemical substance. If the keratoma on the skin does not hurt, there are no seals inside it, this is considered normal. Prolonged exposure to the scorching sun increases the risk of tumor formation. But you can sunbathe in the summer during the period when the sun is least aggressive (before 11 and after 15 hours).
Keratomas can appear as a result of a malfunction in the body. This is due to a deficiency of vitamins and microelements, hormonal imbalance, and metabolic disorders. Such neoplasms often develop in people after 30 years of age. Age-related changes affect the skin, it becomes dry, inelastic and susceptible to the appearance of keratomas. Another common cause is a hereditary factor. You should carefully monitor your diet. If a person notices changes in the skin, he should add to his diet foods containing vitamins A and E. The first is found in carrots, apples, sweet peppers, cottage cheese, and eggs. There is a lot of vitamin E in nuts and spinach.