HPV type 39 is a human papillomavirus with a pronounced oncogenic status, which causes the development of a pathogenic process in healthy cells and can contribute to the formation of cancer.
Statistics show that about 95% of women infected with HPV do not detect any traces of the virus within the first two years. Only regular examinations, prevention, protection from risk factors, and increased immunity can prevent and cure the disease.
Human papillomavirus – type 39. How dangerous
Human papillomavirus type 39 belongs to the highly carcinogenic group
HPV can cause less serious growths such as plantar warts, as well as higher risk growths such as genital warts. The risk lies in the degree of oncogenicity - the ability of pathological neoplasms to become malignant and develop into a cancerous tumor.
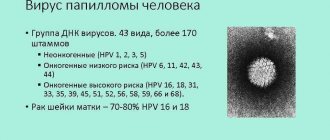
According to the degree of carcinogenicity, three groups are distinguished:
- Non-oncogenic;
- Moderate oncogenicity;
- High risk.
Human papillomavirus type 39 belongs to the latter group and most often manifests itself in the form of flat condylomas on the mucous membrane of the vagina, cervix and cervical canal. In some cases, growths appear on the skin and in the anogenital area (genital warts).
If papillomavirus type 31, 39 is detected in the body, women need an urgent examination by a gynecologist with further tests to effectively diagnose the disease.
In men, this strain of the virus rarely causes external symptoms in the form of growths - they are often carriers of HPV.
How is HPV type 39 transmitted and manifested?
Modern medical science has identified more than 150 types of virus. Depending on its type, it affects the functioning of all organs and systems of the human body. For example, infected people notice various new growths on their skin and mucous membranes in the form of condylomas and wart-like growths.
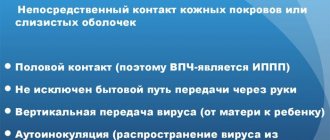
The main route of transmission is physical contact with a carrier, including sexual intercourse without a condom. But household infection is also quite common.
Usually, after entering the body, the infection does not manifest itself in any way, so people do not even know that they are carriers.
DIAGNOSTICS
When diagnosing the disease, self-examination can help - regularly examining your body for the appearance of warts or atypical growths. Detection of condylomas, papillomas on the arms, legs, face and genitals is a reason for examination by a doctor.
Basic diagnostic methods:
- clinical examination;
- examination and examination by a gynecologist “in the mirror”;
- colposcopy;
- biopsy, histological examination - reveals thickening of the stratum corneum;
- cytological examination of cervical smears using the PAP method to identify atypical cells;
- PCR typing – identifies HPV DNA;
- Digene screening test is a modern and highly accurate diagnostic method for identifying the maximum concentration of HPV;
The data obtained during the examination will help determine the type of pathogen, identify the type of virus and the degree of concentration in the body. Depending on the diagnostic results, treatment is prescribed.
Cervical cancer and HPV 39
Cervical cancer is one of the few types of malignant neoplasms for which the underlying cause of the disease has been established. Numerous studies have shown that human papillomavirus DNA is found in almost all cases of precancerous conditions and cervical cancer. Infection with the papilloma virus precedes subsequent squamous (scaly) intraepithelial dysplasia of the cervix.
The third stage of cervical intraepithelial neoplasm occurs only in the presence of persistent infection with high oncogenic risk papillomavirus genotypes.
It has been proven that long-term persistence (5–10 years) of papillomavirus genotypes of high oncogenic risk in women over 30 years of age is associated with a significant increase in the risk of developing malignant changes in the cervix. Infection with papillomavirus genotypes of low oncogenic risk can clinically manifest itself in the form of genital warts.
| Classification of HPV types according to the risk of oncogenicity (Lorincz I, 1992). | |
| Risk category | HPV subtype |
| high | 16, 18, 45, 56 |
| average | 30, 31, 33, 35, 39, 51, 52, 58, 66 |
| short | 6, 11, 42, 43, 44, 53, 54, 55 |
HOW CAN YOU GET INFECTED?
Men and women with active sexual lives are at risk of contracting HPV at any point in their lives if they do not take precautions. In men, the virus practically does not manifest itself, but in women, if untreated, it causes cervical dysplasia.
The human papillomavirus can be infected through household contact, sexual contact, or through contact with infected semen or vaginal secretions.
The best method of protection during sexual intercourse is a barrier method, using a condom. However, this method of contraception cannot protect against contact with other infected areas of the body. Promiscuous sexual relations and frequent changes of partners are an increased risk factor for HPV infection.
It is also possible for household infection through touch, tactile contact, household items, and hygiene products. The virus is able to live for some time in humid environments: baths, saunas, swimming pools, gyms. It can enter the body through injured skin: abrasions, scratches, cuts, as well as during shaving and hair removal.
Signs of HPV in women
In women, human papillomavirus infection can cause the appearance of genital warts - genital warts.
In women, human papillomavirus infection can cause the appearance of genital warts - genital warts, which in many cases are detected only during a gynecological examination.
They grow approximately three months after infection. Most often they form on the labia minora, in the vagina, on the cervix, cervical canal, and on the skin around the anus.
Externally, they are small formations that are located on a wide “leg” and have uneven edges. However, the types of HPV that cause genital warts are not the types that cause cancer.
Symptoms of the disease in women also include cervical intraepithelial neoplasia, a precancerous condition of the uterine mucosa that causes impaired cell maturation. At the moment, doctors know three stages of this disease, two of which are not particularly dangerous, and the third is the first stage of cervical cancer. Viruses types 16 and 18 cause similar symptoms. Cancer is also provoked by types 31, 33, 35 and 39.
Symptoms of HPV in both women and men can include the presence of small growths not only on the genitals, but also in other places - under the breasts, in the armpits, on the neck and on the eyelids.
For men, the disease is less dangerous than for women. And if some carcinogenic types of the virus, which cause the development of growths on the skin in men, rarely provoke tumors in the stronger sex, then a woman, having become infected with them from a man, runs the risk of developing cervical cancer.
Specifics of the course in women
The infection can occur in a latent form, or can cause the development of genital papillomas. Genital warts are observed mainly in women aged 15 to 30 years. The risk of condylomatosis is 10% in sexually active women. It is advisable to be tested for the presence of the virus from 26 to 28 years of age. At the same time, having contracted the virus in her youth, a woman may not suspect it for decades.
And only at the onset of menopause can the virus cause malignancy of the cells of the genital mucosa. The main danger of developing a disease caused by types 16 and 18 is the development of cervical cancer. Cervical cancer reduces life expectancy by an average of 26 years. From the point of view of cancer development, only the virus that remains in the body for more than a year becomes dangerous. Therefore, regular examination by a doctor can prevent all negative consequences.
Causes of infection
Infection with HPV type 35 occurs mainly through sexual contact. However, it can be spread by using toiletries, kissing and touching.
As a rule, with a sufficiently strong immune system, the infection is suppressed by the body itself, and further development does not occur.
The incubation period for the disease lasts from six months to several years. The virus begins to appear and become active under favorable conditions:
- smoking;
- hormonal imbalance in the body;
- infection with sexually transmitted infections and especially genital herpes.
Most often, the virus can be found in the urethra, seminal fluid, and prostate secretions.
The development process from infection to the appearance of a cancerous tumor can last up to 30 years. Degeneration into a malignant tumor does not occur a year after becoming infected.
The risk of infection appears:
- at the onset of sexual activity in adolescence;
- with a large number of sexual partners;
- with inattention to your own health;
- in cases of advanced cervical erosion, weakened immunity.
Course of HPV 39
The disease occurs in four stages:
- Stage 1 – latent course . The virus is present in the body, without causing any changes in cells and without manifesting itself in any way. In this form, it can only be detected by a special PCR analysis.
- Stage 2 – clinical signs appear. The virus causes an acceleration of epidermal cell division. Growths appear on the skin. At this stage, the virus can be detected using PCR, as well as cytology and histology (the presence of hyperkeratosis is determined).
- Stage 3 – dysplasia. The DNA of the virus interacts with the DNA of cells and the so-called integrated form develops. The structure of cells changes. This phenomenon is called koilocytosis. All of the above diagnostic methods are used, as well as colposcopy.
- Stage 4 – carcinoma. Integration of the virus provokes cell mutations and the appearance of malignant cells. Invasive cancer develops. Diagnosis is carried out by clinical manifestations, as well as using all the previously listed methods.
How to identify HPV genotype 39 - diagnostic methods
The presence of HPV strain 39 DNA is determined using the PCR method (polymerase chain reaction)
Diagnosis begins with examining a woman on a gynecological chair using a mirror. Qualified specialists perform colposcopy (using a microscope to examine the walls of the vagina and cervix). Then cytology is performed - the study of separately selected biological material (helps to identify oncology at the initial stage).
The presence of HPV strain 39 DNA is determined using the PCR method (polymerase chain reaction). The disadvantage of this procedure is the impossibility of determining the body’s viral load, which is very important for correct diagnosis and prescribing an effective course of treatment.
The number of HPV type 39 particles is determined using a more modern procedure - the Digen test. For additional information about the condition of the cells, a biopsy (examination of tissue material from the cervix) may be done. Histological studies are also carried out.
Digene HPV test
The Digene HPV test is a molecular technology from Digene, protected by international patent law, aimed at identifying specific DNA fragments of the human papillomavirus (the “hybrid capture” method).
The Digene HPV test makes it possible to differentiate between 2 groups of virus genotypes - high and low cancer risk. Test No. 394 detects the presence of HPV DNA of a group of high-risk genotypes (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68). Test No. 395 detects the presence of HPV DNA of the low-risk genotype group (6/11/42/43/44).
The Digene HPV test is widely used due to its reliability and ease of use. The sensitivity of the test in combination with cytological examination in detecting precancerous changes of the cervix and cervical cancer is much higher than performing cytological examination alone.
It is considered advisable to perform a Digene HPV test if the results of the PAP test are indeterminate. Currently, the combination of the Digene HPV test and the cytological PAP test is becoming the “gold standard” in this area of diagnosis and is proposed for screening women over 30 years of age. The method is standardized. This is the only FDA-approved high-risk HPV detection test. The test was approved by the Federal Service for Supervision of Healthcare and Social Development of the Russian Federation.
The Digene test detects a clinically significant level of infection with the human papillomavirus, leading to the development of cervical neoplasia (in contrast to conventional PCR methods aimed at maximum sensitivity for detecting viral DNA, which does not always have direct clinical correlations). A positive Digene HPV test in women under 30 years of age is an indication for retesting after 9 months, since HPV infection may be transient in younger women.
A positive Digene HPV test in women over 30 years of age may indicate persistence of the virus. With a corresponding result of a cytological study, this means that the woman has a high risk of developing cervical cancer and requires special prevention or treatment. Modern treatment methods make it possible, if detected early, to dramatically reduce the incidence of cervical cancer and especially its incurable cases. Testing for the presence of the virus after treatment allows you to verify its effectiveness.
Treatment of HPV type 39
The effect of laser on condylomas
Scientists have not yet developed a drug that would destroy the structure of the virus. Doctors use some therapies that inhibit the growth and development of HPV and prevent its reproduction, so that the population does not provoke intraepithelial pathological growths.
To suppress papillomavirus strain 39, treatment must be combined and include the following types of therapies:
- Destructive;
- Immunocorrective;
- Antiviral;
- General strengthening.
First, the growths must be removed by chemical methods (caustic substances) or physical methods (laser, radio wave, electrical excision, cryogenic).
Growths caused by HPV strain 39 are most often removed with a laser device, since it leaves virtually no traces or scar tissue, which is so undesirable for the mucous membrane of the vagina and cervix. Large malignant growths are excised with a scalpel, trying to cover as large an area as possible.
To prevent papillomavirus type 39 from causing growths to reappear, antiviral and immunostimulating therapy is carried out. Preparations can be for local transdermal use in the form of ointments, suppositories, or for general use (injection solutions, tablets).
For example, to increase local immunity, a specialist may prescribe interferon inducers in the form of ointments and creams (Cycloferon, Viferon), as well as antiviral drugs for parenteral (Panavir) and oral use (Groprinosin).
After entering the body, the virus can take root, or it can be eliminated on its own after some time - it all depends on the state of the immune system.
Symptoms of infection
In many cases, when faced with the human immune system, the infection is destroyed or suppressed, so that the course and development occur asymptomatically. However, in some cases, when the body fights the virus, symptoms such as:
- temperature increase;
- the appearance of itching and irritation in certain areas of the skin;
- development of a febrile state.
You can understand that the virus has begun to develop and has not been stopped by the body when small pinkish papillomas on a thin stalk appear on the woman’s genitals. The same can be observed on the male organs.
It is additionally important to know that infection can also occur in young children if the mother was infected during pregnancy. The child has a high risk of infection during the birth canal. In such cases, a caesarean section is used.
Papillomavirus type 39 - how to protect yourself from infection
In foreign medical practice (not so popular in domestic practice), adsorbed recombinant vaccines Gardasil and Cervarix have been used for ten years.
In foreign medical practice (not so popular in domestic practice), adsorbed recombinant vaccines Gardasil and Cervarix have been used for ten years. They contain empty shells of the virus, which, when they enter the body, cause the production of antibodies - this is how stable immunity to HPV 16, 39 and other strains is formed.
In the instructions for the vaccines, the manufacturer indicated that they are active only against HPV types 16 and 18, but doctors claim that immunity is developed to all strains of the virus. It is also stated that the protection is formed for 10-15 years, but in practice it is quite longer.
In order to reduce the number of cases of cervical cancer and precancerous conditions (late-stage dysplasia), which are caused by HPV strains 31 and 39, almost all women aged 9-25 years are vaccinated.
The vaccine can be used at any age - there are no restrictions, there are recommendations. The sooner Gardasil or Cervarix enters a woman’s body, the more stable immunity will develop. Vaccines do not destroy the DNA of the virus if the vaccination was given while the strain was in the body.
Life after treatment - basic rules of prevention
If you manage to stop the activity of the virus, it is recommended to adhere to a number of rules, including the following:
- frequent change of sexual partners is a risk factor that provokes infection, which means it should be excluded;
- Condoms must be used during sexual intercourse.
In addition, it is important to maintain intimate hygiene. Additionally, you should follow recommendations that help improve immunity. HPV is difficult to eradicate, but it can be kept dormant for long periods. This makes it possible to reduce the risk of developing warts on the skin.
HPV vaccine
Depending on the vaccine, vaccination occurs immediately against the most dangerous types of HPV. The vaccine is not live, so it is completely harmless. The types of viruses that the vaccine is effective against can cause cancer of the vagina, cervix, penis and anus.
There is evidence that vaccination also protects against a number of other oncogenic types of the virus. The vaccine cannot be used as a treatment, but only as a preventive measure.
There is no need to undergo any special examinations before vaccination. Vaccination is given to young people of both sexes aged 9 to 17 years, and women up to 26 years old. Research is being conducted on the effectiveness of vaccination among older women.
Indications:
- Prevention of cervical cancer,
- Prevention of cancer of the vagina, vulva, penis in men,
- Prevention of genital genital warts,
- Prevention of precancerous diseases,
- Prevention of laryngeal papillomatosis.
How is vaccination carried out?
The effectiveness of vaccination ranges from 95 to 100%
The vaccination is done three times. The interval between the first and second is two months, between the second and third is four months. But you can also do it according to a more dense scheme: the second one a month later and the third one two months after the second one. If all three vaccinations have been carried out within 12 months, it is successful and complete. The effectiveness of vaccination ranges from 95 to 100%.
Side effects of vaccination
In isolated cases, there was a deterioration in health in the first three days after vaccination, and a slight increase in body temperature. The vaccine injection site turns slightly red. Contraindications: Absolute: Individual intolerance to vaccine components (including aluminum or yeast). Relative: Diseases in the acute stage, including exacerbation of chronic ones. Vaccination can begin after the exacerbation has ended or the patient has been cured.
Sources:
- https://www.invitro.ru/analizes/for-doctors/554/2734/
- https://www.hpvinfo.ru/papillomavirus/infection.html
- https://www.onclinic.ru/articles/zabolevaniya/polovye_infektsii/simptomy_vpch_u_zhenshchin/
- https://www.zppp.saharniy-diabet.com/papillomy/tipy/onkogennye/39-tipa
- https://www.tiensmed.ru/news/virus_papillomy_chjelovjeka.html