Reasons for HPV activation
HPV type 56, as well as other strains of the virus, enter the body through microdamages on the skin or mucous membranes. After penetration, the infection takes root and takes root in the epithelial layer without any visible manifestations - the course of the disease is latent. This happens as long as the immune system is able to suppress the activity of the papillomavirus (the incubation period can last several years).
Important! Even such a latent presence of type 51, 56 infection in the human body can be dangerous for surrounding people - close bodily contact with the carrier entails infection.
The presence of any unfavorable factors, be it exacerbation of chronic ailments, frequent stress, STDs, reduce the protective barrier - the immune system weakens, and HPV becomes more active. Now the infection is fully manifested and the first symptom is the formation of single genital growths (condylomas).
Also, quite often the manifestation of papillomavirus can be observed in pregnant women - this is the result of unstable hormonal levels. It is important to carry out treatment before the baby is born in order to prevent its infection during passage through the birth canal.
HPV can become more active with the onset of menopause. During this period, the female body is saturated with estradiol (a derivative of the hormone estrogen), which stimulates the vital activity of human papillomavirus infection.
Preventive actions
Since no medicine kills HPV, and only a healthy body can cope with this task, measures must be taken to strengthen the immune system. To do this, it is recommended to eat right, follow a daily routine and avoid stress.
Sexual contacts should be protected whenever possible, but it should be remembered that barrier contraception does not provide 100% protection against HPV, since the condom may not isolate all contacting areas of damaged skin, and the virus particles are very small in size.
Vaccination against the virus is given to children aged 10-12 years before puberty. This primarily concerns girls, since HPV penetrates the female body more often, but to prevent the circulation of the harmful agent, it is recommended to vaccinate boys as well. For adults, vaccination does not help develop immunity, so it is used only if HPV has already been diagnosed.
It is very important to pay attention to neoplasms, since they tend to become malignant. Early detection of viruses, treatment of the consequences of their impact on the body and taking measures to increase immunity significantly increase the chances of preventing unpleasant consequences.
Danger of viruses 51 and 56 types
We have already said that hpv genotypes 51 and 56 are included in the group of increased oncogenic risk, so treatment should be done at the first signs of pathology.
Without adequate therapy, the infection progresses, single condylomas merge into one single conglomerate. Viral DNA not only infects the cavity, but begins to integrate into the chromosomal compartment of the cells, and their transformation (mutation) occurs. The result of this activity is the proliferation of atypical cells that are inherent in malignant tumors.
HPV 51, 56 are anogenital infections, so they can cause cancer:
- Women usually develop oncological processes on the cervix and vulva;
- In men, the penis and prostate suffer, and in the presence of homosexual relations, damage to the rectum is possible.
In addition, activation of the virus 51, 56 affects the reproductive sphere - in advanced cases it causes infertility or can cause spontaneous abortion (miscarriage).
It should be noted that it is no longer possible to cure HPV for a person who has crossed the 30-year mark; it is a chronic disease, so he should learn to live and keep the virus in a latent state. It is also important to consult a doctor at the first signs of pathology development.
Human papillomavirus (6,11,16,18,31,33,35,39,45,51,52,56,58,59,68) (quantity)
Human papillomavirus (HPV ), Human papillomavirus (HPV) belongs to the papovaviridae family, a genus of papillomaviruses. This is a DNA-containing small virus, heat-stable. It is the most common sexually transmitted infection: according to some data, up to 80% of the population is infected at a young age. The virus exhibits affinity for the epithelium of the skin, mucous membranes of the genitals and other organs (larynx, oral cavity, conjunctival mucosa).
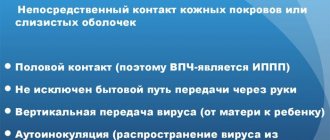
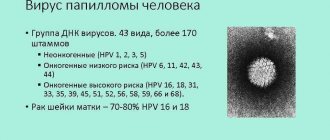
The main route of transmission is sexual contact, including anal and oral sex; unfortunately, the use of condoms does not protect against infection with this virus. Transmission is possible through close contact of skin and mucous membranes with infected areas. An important factor in infection of a newborn with the subsequent development of respiratory papillomatosis of the larynx is infection during passage through the genital tract during delivery. Today, more than 100 types of human papillomavirus (HPV) are known, and more than 40 of them can cause damage to the anogenital tract (genitals and anus) of men and women and the appearance of genital warts. Papillomaviruses can be divided into 3 main groups:
- non-oncogenic HPV (genotypes 1, 2, 3, 5);
- low carcinogenic risk (LCR) HPV (6, 11, 42, 43, 44 genotypes);
- high carcinogenic risk (HCR) HPV (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68 genotypes).
HPV of low carcinogenic risk (HPV NKR): a group of viruses that leads to benign lesions is represented by 5 genotypes, but the main ones are 6 and 11, which account for up to 90% of all cases of infection with these viruses. The most common clinical manifestation of NCR HPV is genital warts (Condylomata acuminata). There are also other types of genital warts: keratotic warts localized on dry skin, papular warts localized on completely keratinized epithelium, giant Buschke-Levenshtein condyloma (found in patients with reduced cellular immunity or during pregnancy). Endourethral condylomas are localized in the urethra, are often combined with ordinary condylomas and are found predominantly in men. Cervical condylomas are often combined with genital condylomas: exophytic condylomas, endophytic (flat).
HPV of high carcinogenic risk (HPV HCR): the group of types of high carcinogenic risk is represented by 15 genotypes, the most common of which are ten: 16, 18, 31, 33, 35, 39, 45, 52, 58, 59. At the same time, the share of 16 and 18 types account for 70% of all cases of infection, and it is these types that are characterized by a high carcinogenic potential; in relation to the 18th genotype, a high frequency of detection is observed in adenocarcinomas. To date, the role of HPV has been proven in the development of cervical cancer, a large proportion of anal cancer (about 90% of cases), about 40% of all cases of cancer of the vagina, vulva, penis, 10–15% of cases of cancer of the oral cavity and larynx.
Viral DNA can persist in the cell in two forms: episomal (productive stage) and integrated (integrated stage). At the episomal stage, increased production of new viruses occurs, which contributes to the involvement of new cells in the pathological process, however, the cells do not lose control over the processes of apoptosis and this stage is characterized by benign changes in the epithelium. The integrated stage is the stage when the virus is integrated into the cell genome and leads to overexpression of oncoproteins E6, E7, is associated with precancerous changes and requires appropriate treatment tactics for the patient.
The infection caused by the human papillomavirus has a number of important features, without which the use of HPV testing is associated with a number of difficulties in interpreting the results.
On the one side:
- HPV is the most common STI (up to 80% of young people are infected with this virus);
- When infected, most women (about 80%) are cured of HPV within 9–15 months from the moment of infection without undergoing treatment procedures (i.e., if the genotyping test is repeated a year later, the previously identified HPV genotype may disappear or the spectrum of genotypes may change). With age, the ability to self-eliminate significantly decreases;
- HPV infection and disease are NOT SYNONYMS! The infection leads to the development of precancer in a small proportion of infected women (about 0.5%);
- On average, 10–20 years pass from infection to the development of precancer and cervical cancer. With age, the ability to eliminate the virus decreases, and accordingly, the risk of developing precancer and cancer increases;
- There are no effective treatment methods at the stage of latent infection (no changes in the cytological and/or colposcopic picture, but the virus is detected).
On the other side:
- HPV is the leading cause of cervical cancer. Infected women have a 300 times higher risk of developing cancer. Not only methods of secondary prevention have been developed (cervical screening to identify precancerous stages), but also primary ones - vaccination of girls and boys aged 9–12 years;
- the infection is insidious and quite often does not cause any complaints in the patient and is not detected during examination until it reaches the stage of invasive cancer;
- clinical manifestations of high-risk papillomavirus infection may be masked by other diseases of the urogenital tract, which does not allow them to be detected in a timely manner using traditional methods.
From the listed features of human papillomavirus infection it follows that:
1. A positive test result for the presence of the virus should be interpreted as:
- the patient belongs to a high-risk group for developing cervical cancer;
- the need for additional thorough diagnostic procedures to determine the current stage of infection, exclude severe dysplasia and cervical cancer;
- the need to monitor infection (persistence) in the absence of clinical or subclinical manifestations.
2. A negative test result is interpreted as no risk of developing severe dysplasia and cancer.
Laboratory diagnostics. Diagnosis of HPV infection is determined by clinical manifestations and clinical tasks of predicting the risk of developing HPV-associated malignant neoplasms.
Laboratory methods for diagnosing HPV infection:
- direct methods: assessment of the presence of koilocytes in cytological smears (low diagnostic sensitivity); detection of the presence of proliferation markers p16/ki 67; molecular methods (PCR analysis), which are carried out in the format of qualitative and quantitative testing with the possibility of genotyping, determination of NCR and HCR HPV genotypes;
- Serological methods are not used to diagnose HPV infection.
Strategies for using HPV tests in the diagnosis of precancer and cervical cancer:
- included in the cervical screening complex: as a triage test for pathological PAP tests in women under 30 years of age; test together with a cytological examination for all women over 30 years of age. In this case, the presence of HPV infection (especially genotypes 16 and 18, with a high viral load) allows us to predict a high risk of having or developing cervical cancer, which determines the need for additional examinations. In case of negative HPV testing results, the screening frequency can be increased to 3–5 years (different recommendations apply in different countries), provided there are no changes in the cytological examination;
- recommended in some countries as a primary screening test for CC in women over 30 years of age;
- monitoring the effectiveness of treatment for dysplasia (the first study is carried out 6 months after treatment together with a Pap test). Moreover, in case of receiving positive results of the HPV test and normal cytology, additional examination is necessary, since the risk of the presence or development of pathology is high.
Various methods of molecular diagnostics (PCR analysis) allow solving various diagnostic problems:
- a qualitative format allows you to detect the presence of infection, but does not allow you to assess clinically significant amounts of the virus, which are associated with a high risk of precancerous lesions;
- The quantitative format allows you to identify the virus and determine the viral load. This makes it possible to assess not only the degree of risk, but also the possible presence of precancerous changes, since a high viral load is associated with the realization of the oncogenic potential of the virus. With correct and standardized collection of clinical material, the viral load is less than 105 genome equivalents (GE) of HCV HPV in a scraping (Josefsson et al, 2000; van Duin et al, 2002; Dalstein et al, 2003; Snijders et al, 2003; Moberg et al, 2004, 2005) or 103 GE per 100 thousand human cells is considered clinically insignificant, since it practically does not occur in severe dysplasia and CC, and is also associated with a minimal risk of their development. On the contrary, the amount of virus more than 105 HE per 100 thousand cells with the established fact of persistent infection (HPV has been detected for more than 1 year) is designated as an increased HPV load and is associated with an increased risk of developing severe dysplasia and is more common in CC. Finally, viral load monitoring provides some information. Thus, it is believed that a decrease in the amount of HPV DNA by more than 1 lg may be a marker of transient infection. Increase in viral load after 3, 6 and 9 months. after treatment indicates the possibility of relapse.
HPV genotyping provides additional opportunities to determine the prognosis of the disease. The need for genotyping can be justified because:
- detection of several genotypes of the virus is associated with a less favorable prognosis of the disease and a higher risk of persistence;
- The degree of oncogenicity of different high-risk genotypes is not the same. HPV types 16 and 18 have the greatest oncogenicity; there are recommendations for determining these two genotypes of the virus after testing for a wide range of types in order to more aggressive patient management tactics: when genotypes 16 and 18 are identified, it is recommended to immediately conduct a colposcopic examination; when other high-risk types are identified - perform cytology first, and only if the cytology result is positive, perform colposcopy;
- Genotyping makes it possible to distinguish reinfection from persistent infection during the patient’s return visit. It is all the more important to receive such information, since it is the chronic persistent form of infection that poses the danger, while recent infection most likely resolves spontaneously. Reinfection is indicated by a change in the spectrum of genotypes; persistent infection is indicated by the persistence of the virus genotype a year after the first testing; re-infection with the same genotype of the virus after self-cure is almost impossible.
Symptomatic manifestations
The first sign indicating activation of HPV in both men and women is the formation of small yellow-gray or pinkish growths in the anogenital area. Without qualified therapy, the neoplasms grow, merge, their surface becomes bumpy and resembles cauliflower inflorescences.
In men, the disease is somewhat milder than in women - condylomas form on the surface of the penis, which over time can spread throughout the entire anogenital zone. In advanced cases, the infection affects the urethra, which may be accompanied by pain when urinating.
Routes of infection and risk factors
The disease is characterized by the appearance of foreign growths on the mucous membrane of the oropharynx, genitals, and skin. The pathogen progresses in the body constantly. Papillomavirus is transmitted in the following cases:
- sexual contact;
- with saliva through the oral cavity;
- in the presence of a wound surface and contact with the affected area;
- from sick mother to child.
The main route of infection is sexual. Moreover, the frequency and timing of sexual intercourse do not affect the entry of the pathogen. The gates of infection are the vagina, cervix, glans penis, urethra, and mucous membrane of the oropharynx.
Factors that provoke infection with the virus:
- decreased immunity as a consequence of the acute inflammatory process of a chronic disease;
- hormonal disorders. Cervical neoplasms depend on estrogen saturation. Pathology develops during pregnancy, menopause, and taking hormonal medications;
- bad habits;
- early onset of sexual activity;
- presence of cancer in relatives.
Diagnostic methods
To identify viruses of types 51 and 56, the following studies are carried out:
- Polymerase chain reaction - any biological fluid is suitable for analysis. The test helps identify the pathogen strain;
- Digen study – determines the serotype, viral load and degree of oncogenicity of HPV;
- Cytological and histological examination is carried out to identify atypical cells.
Primary diagnosis is also important - examination by a gynecologist, colposcopy in women and visual urological examination in men.
A positive test result for HPV 51, 56 implies mandatory drug treatment, as well as destruction of pathological growths.
Important! Several types of highly oncogenic HPV can be present in the human body at the same time. This proximity increases the risk of developing malignant neoplasms.
The importance of prevention
A person can live with papillomavirus type 51 all his life and never know about it. Doctors recommend that people under thirty years of age be tested for HPV. In some cases, if the virus is present in the body of people under 25 years of age, a strong immune system can contribute to its elimination (self-destruction). But often the microorganism remains and, under favorable conditions, begins to multiply.
To prevent infection with HPV type 51, you need to completely abstain from sexual relations, but since this task is difficult to accomplish, preventive measures should be followed. Experts recommend:
- lead a healthy lifestyle, play sports;
- undergo regular examinations to detect the virus;
- promptly treat existing diseases, including STIs;
- Begin sexual activity no earlier than 18 years of age;
- try not to terminate pregnancy using artificial methods;
- reduce the number of sexual partners, settling on one, more reliable one;
- Remember that a condom is not a reliable method of protection.
Vaccination is considered a reliable measure to prevent the development of HPV. For this, two drugs are used: Gardasil and Cervarix, which, according to reviews, are absolutely harmless.
Complex therapy
To date, there are no medications that would completely remove HPV from the body. However, with adequate antiviral therapy, the concentration of the virus can be significantly reduced; for this purpose, medications such as Groprinosin, Cycloferon, Allokin-alpha, Panavir, and others are used.
Since serotypes 51 and 56 have increased oncogenicity, patients can be prescribed cytostatics - Podophyllin, Bleomycin, 5-fluoroene, Vinblastine, which prevent the growth of malignant tumors.
What to do next
If you have been diagnosed with HPV type 51, 56, complex therapy is mandatory, after which you must follow precautions throughout your life:
- Regularly undergo preventive examinations;
- Do not neglect the rules of personal hygiene;
- Streamline sexual relations;
- Use contact contraception;
- Saturate your diet with healthy foods;
- Take a course of vitamin therapy at least twice a year;
- Give up bad habits - in general, lead a healthy lifestyle.
Your main task is to strengthen and increase the body’s supporting forces. Since HPV is an immune-dependent virus, whether you will have a relapse or not directly depends on the state of your immunity.
Treatment
Papillomavirus 51, like all types of HPV, cannot be treated.
If you have a strong immune system, the body can heal itself. But these isolated cases are the exception, not the rule. Each individual case of the disease requires a special approach, taking into account the clinical picture, the general well-being of the patient and the presence of concomitant chronic processes. Firstly, all condylomas on the skin and mucous membranes are removed. To do this, one of the methods can be used:
- cryodestruction – burning with liquid nitrogen;
- electrocoagulation;
- laser removal;
- radio wave;
- surgical removal;
- cauterization with chemicals.
Secondly, to help the body get rid of the pathogen, antiviral and antitumor therapy is carried out.
Thirdly, they strengthen the body's defenses. To do this, together with taking immunomodulators and multivitamins prescribed by the doctor, follow a daily routine, monitor proper nutrition and harden yourself.
On the recommendation of a doctor, the main therapy can be supplemented with folk remedies that enhance immunity.
- Mix lemon balm, nettle, horsetail, plantain, wormwood, violet and dill in equal proportions. 4 tbsp. collection, pour 800 ml of water and put on fire. The infusion should boil for 10 minutes and then infuse for 2 hours. After this, it is filtered and taken 3 tbsp. l. before eating.
- Freshly prepared pink potato juice is taken 100 ml morning and evening, 30 minutes before. before meals. The course lasts 2 months.
- Multivitamin mixture. All ingredients are taken in equal quantities. Grind cranberries, walnuts, dried apricots and lemons. Add honey to the resulting mass and mix. The product is taken immediately after meals, 2 tbsp. l.