An HPV smear is a test of biological material to determine a viral infection. The procedure for identifying the human papillomavirus is carried out for women and men to determine the type of pathogen and the degree of oncogenic danger. When diagnosing HPV, a smear procedure is required; the indicators affect the examination result and further treatment tactics.
Symptoms and first signs of the disease
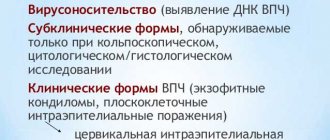
Even after entering the human body, human papilloma viruses may not manifest themselves at first. When immunity decreases, the virus is activated and begins to multiply. At this stage, clinical manifestations appear.
When infected with HPV of low oncogenic risk, patients are most often concerned about visual discomfort associated with the appearance of warts on any part of the skin and mucous membranes. These formations in the anogenital area have a special name - genital warts or anogenital warts. They are often accompanied by itchy skin. As a rule, these formations are of various shades of brown, have an uneven surface, and may be on a narrow base (leg).
Appearance of skin warts
A distinctive feature of warts and condylomas is rapid and multicentric growth. The presence of single warts on the skin and mucous membranes is an indirect sign of HPV infection and requires diagnosis.
Most infections caused by highly oncogenic types of HPV are asymptomatic. Only a general decrease in immunity is possible. Often the virus can only be detected after swab collection. However, the prolonged presence of an oncogenic type of virus leads to the development of precancerous pathologies, which, without appropriate therapy, degenerate into a malignant process. It is well known that in the early stages of the disease, cervical cancer is practically asymptomatic, and specific manifestations (discharge and irregular bleeding, pain in the back, pelvis, legs; unilateral swelling of the legs) occur when the process is widespread.
Viruses of high oncogenic risk - HPV 16, 18, 31, 33, 39, 50, 59, 64, 68, 70. The most studied and aggressive are types 16 and 18; these HPVs in women cause up to 70% of all cases of precancerous conditions and cervical cancer.
Is screening reliable?
HPV screening is a complex procedure that combines several options for laboratory tests, the combined use of which makes it possible to determine the presence of pathogenic flora in the body, the type of infection, as well as the viral load. To obtain more informative results, a double application of this diagnostic procedure is required.
If, after the initial examination, the papilloma virus is detected in significant quantities in the patient, appropriate treatment is possible. After therapeutic procedures, repeat HPV screening is required. If the infection is detected again, there is a possibility of developing a malignant tumor; of course, this is only possible against the background of invasion by strains of the virus with high oncogenic activity.
Diagnosis of HPV in women
The polymerase chain reaction method, the so-called PCR, can reliably identify a specific type of papilloma virus. For analysis, a vaginal smear into a test tube with a special medium is sufficient. PCR is a simple but highly sensitive method.
A positive test for HPV 16 and 18 is associated with a higher risk of malignancy.
Eppendorf tube for collecting material for HPV testing
It is important to understand that changes in the cervix are often not visible to the naked eye, so it is necessary to use special additional examination methods, such as colposcopy and smears from the cervix and cervical canal.
Colposcopy is an examination of the cervical mucosa using a special device - a colposcope.
In this case, 2 tests are carried out:
- Acetic Acid Test - test with acetic acid solution
- Schiller's test - treatment of the surface of the cervix with Lugol's iodine solution.
Based on the data obtained, a satisfactory or unsatisfactory colposcopic picture is judged. This test is performed using a special Papanicolaou stain, which is why it is often referred to as a PAP test.
Detection of a pathological type of smear and an unsatisfactory colposcopic picture are indications for a biopsy of suspicious lesions.
Pap smear staining
What can affect the reliability of the results?
HPV is dangerous, but does not mean that a positive test result indicates the presence of cancer. Sometimes research results have unreliable data. May affect:
- human factor. The laboratory assistant may make a mistake during research;
- contamination of the patient’s biological material distorts the smear result;
- use of contraceptives or other medications during testing;
- storage conditions for biological samples were violated;
- using the wrong method to study the material;
- the inability to detect viruses in the body using existing medical equipment;
- comparatively small amount of viruses contained in the sample.
Infectious infection occurs simultaneously with several types of viruses. It is difficult to accurately determine the presence of certain problems. Experienced doctors prescribe a comprehensive examination to patients, consisting of several diagnostic methods, which allows them to obtain reliable results.
Prevention and treatment
The issue of preventing human papillomavirus is currently being actively discussed.
Patients often ask, is there a vaccine for cervical cancer?
In fact, there is no such vaccine. There is no treatment for the papilloma virus that would completely remove the virus from the human body. Only the result of the virus’s impact on the body’s cells can be treated. Regimen containing antiviral drugs and immunomodulators are used. The papillomas themselves can be removed surgically: by radio wave techniques, laser coagulation, and also by methods of chemical destruction.
All these types of therapy are actively used on the basis of the National Medical Research Center for Oncology named after N.N. Petrova after a thorough examination, examination and individual selection of treatment by highly qualified specialists. Undergoing therapy in a non-specialized institution may result in the spread of the virus to surrounding tissues damaged during the removal of the affected areas.
Viral load clarification
The possibility of obtaining a quantitative assessment of the concentration of HPV in the smear material is provided by both methods - the real-time PCR option and DIGIN.
However, to analyze a smear for the concentration of papilloma pathogens, some doctors recommend using the DAGIN test. The information has important clinical implications. Since it allows you to assess the activity of HPV replication, response to treatment and the likelihood of relapse of papilloma.
How accurate are the results?
According to the results of clinical trials, the accuracy of molecular biological analyzes reaches 98-100%. This is if we take specificity - the ability of a test system to identify the genotype of a particular HPV in a sample, if they are present. But when it comes to sensitivity, everything is not so clear-cut; the range of values is 65-98%. In other words, the probability of getting a false positive answer is almost zero.
But the chance of a false negative result can reach 35%, which is not so small. Everything is explained simply. The main thing on which the reliability of test results depends is that HPV-infected cells get into the smear. If they are not there, the laboratory will give a negative result for typing and, naturally, for concentration. Such cases, although rare, do occur.
Therefore, in addition to carefully following the procedure for taking a smear, a number of other conditions must be met:
- The smear result becomes positive several weeks after infection. If you take a sample earlier, it is likely to be negative.
- Taking antiviral drugs can lead to false negative results, especially if the condyloma is localized in the mouth. In such cases, a smear should be taken 10-14 days after the last use of the medicine. Antibiotics do not work on HPV; the test can be taken at least an hour after taking antibacterial drugs.
- In case of a doubtful result, the smear should be repeated after a few days using another laboratory test method.
This is what concerns the medical part of diagnosing HPV in condylomas.
Vaccines against human papillomavirus
There are currently 2 recommended vaccines in use. It is considered optimal to vaccinate girls before they become sexually active.
Since 2006, the Gardasil vaccine has been used (Fig. 4). This is a quadrivalent vaccine, i.e. it is directed against HPV types 6, 11, 16 and 18.
The recommended course of vaccination consists of 3 doses and is carried out according to the following scheme: first dose - on the appointed day; the second - 2 months after the first; the third - 6 months after the first. Carrying out the full course leads to the formation of stable immunity in 99% of vaccinated people for a period of at least 36 months in all age groups. Children and adolescents, as well as young women aged 9 to 26 years, are subject to vaccination.
Another vaccine is Cervarix. Created in 2007 for the prevention of diseases caused by human papilloma viruses types 16 and 18. A full course of vaccination according to the 0–1–6 month schedule leads to the formation of specific immunity in 100% of vaccinated individuals 18 months after the last dose of the vaccine in age groups from 10 to 25 years. The need for revaccination has not yet been established.
Vaccines against human papillomavirus a) Gardasil b) Cervarix
In a number of regions of the Russian Federation, patients are vaccinated free of charge, while in others vaccination is carried out on a commercial basis.
Preparation for the procedure
It is best to conduct an examination of the female body in the first half of the menstrual cycle, but not earlier than the 5th day. Research is allowed in the 2nd half of the menstrual cycle, but no later than five days before the start of menstruation.
If there are pronounced signs of inflammatory processes, biomaterial should be collected on the day of treatment. On the eve of the examination and on the day of the examination, a woman should not undergo vaginal douching.
Experts do not recommend taking material during antibacterial therapy, regardless of whether it is local or general. It is also impossible to carry out an important procedure during menses, earlier than 1-2 days after sexual intercourse, colposcopy and intravaginal ultrasound.
It is recommended to take biomaterial no earlier than 2 weeks after using local antiseptics and antibacterial agents, and no earlier than 30 days after using oral antibiotics.
When taking a scraping for examination from the urethra, the collection of biomaterial should be carried out before urination or only after 2-3 hours after urination.
It is advisable to strictly follow all of the above rules, unless other conditions are put forward by the attending physician.
In order to improve the services provided by the laboratory, changes in research execution technologies are possible.
Dynamic observation
Today, cervical cancer screening in the Russian Federation is regulated by Order No. 572n of the Ministry of Health: preventive examinations with cytological screening are carried out at least once a year. PCR testing of vaginal discharge for the presence of human papillomavirus is not prescribed as part of a preventive medical examination. However, according to international standards, HPV detection is an important and integral factor in the prognosis of cervical diseases. Initial HPV testing is recommended, as is cytological screening of the cervical epithelium. The screening interval for patients with a normal cytology test result and a negative HPV test ranges from 1 to 3 years.
Disadvantages of the method
There are, however, some negative aspects in carrying out PCR diagnostics. The main one is the possibility of obtaining a false positive result.
This happens if treatment has already been carried out, the infection has been defeated, but dead cells still remain inside the tissues. Cell renewal takes time.
If the analysis is carried out earlier than 2-3 months, PCR may show a positive result, in fact mistaking already dead cells for living ones.
The method does not distinguish between them; it is aimed at searching for viral DNA, which can be found even in already dead cells. All this leads to a false positive result.
This situation can be avoided if you take the test within the time limit established by your doctor.
There is also a risk of a false negative result. In this case, the patient cannot influence the quality of the diagnosis in any way, since a false negative analysis is a miscalculation of the laboratory. It may occur if:
- the collected material was improperly transported and stored;
- sterility is compromised and other microorganisms get into the samples obtained;
- the reagents were unsuitable.
In order to exclude the possibility of obtaining a false negative result, it is necessary to choose a trusted laboratory with qualified personnel.