Diagnosing cancer at an early stage is very important. The sooner the problem is detected, the faster and better the treatment will be. Scientists and doctors all over the world are fighting this terrible disease and have achieved good results, but they cannot completely defeat it. The discovery of tumor markers was a big breakthrough in this direction, since some of them help not only to detect the presence of a disease, but also to determine its location in the body and even the size of a malignant neoplasm.
On the other hand, there is no ideal tumor marker that would accurately determine the type of cancer. Each time it is necessary to carry out a whole range of tests, including not only blood sampling to identify tumor markers, but also computed tomography, biopsy, x-rays and other studies.
Kidney oncology and skin cancer are the most difficult to diagnose and tests give results only in the later stages of the disease, when metastases have already spread throughout the body. But this does not mean that in these cases tumor markers are useless. An experienced oncologist knows well that they can serve as a signal for a comprehensive examination of the patient.
What are tumor markers
Tumor markers are certain protein or other compounds that are produced by the body in response to cancerous damage to any organ or tissue. Malignant formations can develop in any organs; depending on the classification and composition of the affected tissue, various specific substances, that is, tumor markers, are produced. Some proteins are produced directly by the tumor, others are created by healthy tissues in response to cancer toxins that are carried throughout the body.
Modern medicine counts several dozen cancer markers in the blood and urine. Some specific substances are produced by one organ, for example, CA-15-3 appears only in breast cancer. Other markers react in many organs and may increase slightly even in somatic processes not associated with the reproduction of cancer cells. For example, carcinoembryonic antigen (CEA) increases in cancer of the stomach, intestines, and genitourinary system, and may slightly exceed standard values during long-term chronic inflammatory processes in the gastrointestinal tract and lungs.
Three types of skin cancer
Skin cancer
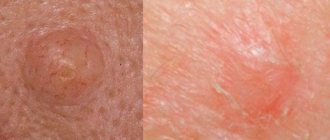
- Basal cell
This is the mildest form, which does not lead to the formation of metastases. It is diagnosed quite simply and treated in the vast majority of cases. Most often it manifests itself in the form of a wound that does not heal for a very long time, up to several weeks, and at times bleeds, itches and hurts. Less commonly, it can take the form of a black, brown, pink or even white mole that slowly increases in size. Basilioma can also be in the form of a scar that suddenly appears without any reason.
- Squamous
It occurs much less frequently, but is also much more dangerous. Diagnosis is more difficult with all the ensuing consequences. It appears as a relatively large pink or white spot or as a wound with convex edges that does not heal for a long time. It can also take the form of a dry and rough spot or the so-called “skin horn”.
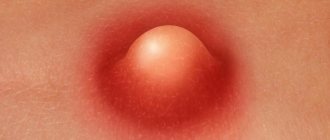
- Melanoma
The most dangerous type of skin cancer. In the early stages it is practically impossible to diagnose, develops rapidly and can lead to death in just a few months. It can be treated only if its initial stage can be determined. You should be concerned if a mole appears on the skin that is different in color, structure and size from the others. Or if one of the old, familiar moles suddenly began to grow quickly.
Squamous cell and especially melanoma are very dangerous and modern treatment methods have great difficulty coping with them. That is why it is necessary to identify their formation as early as possible. Although this is not easy, it is quite possible.
Features of analysis for tumor markers in skin melanomas
In melanoma, tumor markers such as β-2-microglobulin, S100 protein, squamous cell carcinoma antigen, and TA-90 are elevated in most patients.
Beta-2-microglobulin is detected in the blood or urine. Detection of an increase in these indicators is considered an important component of diagnostics in oncology of skin tumors. With diffuse melanoma, this protein increases in 70-80% of patients. However, exceeding the normal range of production of this protein can cause autoimmune and lymphoproliferative diseases. Normal values in a healthy adult range from 0.6-2.3 mg/l in the blood and less than 0.3 mg/l in the urine.
In approximately 30% of patients who have cutaneous melanoblastoma, the S100 protein level increases. This marker is not indicated for primary diagnosis, but for monitoring treatment and assessing early relapses. The marker concentration is determined in serum obtained from venous blood. The amount of S100 protein is considered to be less than 0.1 μg/l.
In squamous cell carcinoma, the parameters of the SCC antigen change. This substance is produced in carcinoma of the skin of the head and neck, cervix, trachea and other organs. Less than 10% of patients with melanoma have elevated levels of this substance. The concentration of this antigen in the blood of healthy people does not exceed 0.2 ng/ml.
Detection mechanism
It is possible to detect the disease in this way due to the fact that the tumor produces special proteins that are abnormal. And it is their presence that is the hallmark of a tumor. The melanoma tumor marker S-100 has been sufficiently studied. Its concentration in the blood and urine is directly dependent on the stage of development of the malignant neoplasm. If it has increased to 70%, the stage will probably be 3rd or 4th. At stage 2 there is much less of it, and at the very initial stage it is minimal and can hardly be detected. For this reason, cancer is called an insidious disease, because it does not reveal itself in the initial stages.
Protein S-100 can also be produced when there is spinal injury. It is also actively released during cerebral hypoxia, myocardial infarction, and bronchial inflammation. Increased concentrations of this protein accompany Alzheimer's disease, stroke, liver failure, and even a number of mental disorders. Therefore, during diagnosis, attention is paid to many factors. It is important to differentiate the diagnosis from a number of ailments.
Often, detecting a protein helps identify disruptions in brain activity before the first clear signs of damage appear.
In what cases is analysis required?
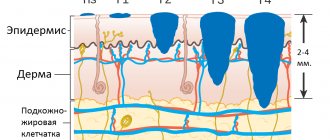
To make a final primary diagnosis of melanoma, a conclusion on histological examination of the affected tissue is necessary. It is the presence of atypical cells and corresponding changes in different layers of the skin that allows us to confirm the diagnosis of a malignant neoplasm.
Based on the increase in cancer markers and clinical manifestations, that is, the presence of dark, diffuse spots on the skin, the doctor makes a presumptive diagnosis. It is written as a diagnosis with a question mark.
Tumor markers are in most cases used for early diagnosis of melanoma relapse. After a skin tumor is removed, abnormal cells may remain in nearby lymph nodes or in underlying tissues. If during the operation all foci of melanoma were not removed, effective chemotherapy and radiation were not carried out, then after a while a new noticeable cancerous tumor will form.
In a body that has already encountered skin cancer, characteristic substances will be produced faster when melanoma re-forms. The sooner a doctor detects a recurrence of cancer, the more encouraging the prognosis for the disease. Therefore, patients who have had melanoma removed are recommended to periodically donate blood for cancer markers. In the first two years after surgery, studies are carried out once every 3 months, then twice a year.
Who needs a melanoma diagnosis and when?
Skin cancer is a tumor that arises from moles that have undergone physical damage due to exposure to other provoking factors. Early examination greatly contributes to the success of treatment of any disease. It is recommended to get tested once a year, especially if you have relatives with cancer. A tumor marker for skin cancer is also required if:
It is recommended to take tests when there is an elevated body temperature that lasts for a long period.
- You constantly feel unwell: weakness, fatigue, pale skin.
- Stable temperature over a long period of time (37.5-38 ⁰C).
- Changes in moles are observed (increase in size, blurring of contours, itching, blood, burning).
- The appearance of a gray-yellow nodule or spot on the surface of the skin.
- When you palpate the base of the tumor, you can feel the tightness of the skin.
- The appearance of a weeping ulcer in the wound.
Preparation for analysis and rules of conduct
Tumor markers are formed in the body over a long period. They accumulate for weeks or months.
There is an opinion that on the eve of the study, food intake, stress, and physical exercise do not fundamentally affect the level of specific substances formed during the cancer process. However, some substances, such as S100 protein, are sensitive to intense muscle work.
In order for the analyzes to give an accurate picture, it is recommended:
- It is best to conduct a blood test in the morning on an empty stomach. It is allowed to take biomaterial for tumor markers 4 hours after eating a light meal. If you take venous blood immediately after eating, then chylosis is possible - an excess content of fatty particles. “Fat” blood is not suitable for research.
- Do not worry. Emotional stress contributes to the destruction of red blood cells, resulting in hemolysis in vitro. Most laboratories do not perform testing from serum with hemolysis.
- Do not smoke 1 hour before donating blood.
- The day before you should not go to the gym or actively engage in physical work.
Urine collection for β-2-microglobulin testing is carried out in a sterile container. In the morning, the patient should empty his bladder into the toilet. Then you need to drink 1-2 glasses of warm water. After about an hour, when you want to go to the toilet, collect the entire portion of urine in a plastic container with a tight lid. Urine must be delivered to the laboratory within 2-3 hours.
How are the tests done?
The procedure for collecting plasma from a vein for tumor markers is carried out on an empty stomach, preferably in the first half of the day.
The melanoma tumor marker is taken in a special laboratory under the direction of a doctor. Blood is drawn from a vein to check for cancer cells. The wait for the results of a laboratory test for melanoma is not long - approximately 3 to 7 days. You should take such tests only if you suspect a skin disease. Rules for taking tests:
- Blood is taken in the morning on an empty stomach.
- The day before, it is advised to eat a light dinner (salad, steamed food, boiled food, baked meat).
- A couple of days before the test, you need to give up alcohol.
- Reduce physical stress on the body on the day of blood collection.
- Do not be nervous.
- Avoid cigarettes before the procedure.
- All medications taken by the patient must be reported to the attending physician.
Return to contents
Standards and decoding
The level of Beta-2-microglobulin in urine is allowed up to 0.3 mg/l; in the blood its concentration in adults should not exceed 2.3 mg/l. However, an increase in this specific protein does not always indicate the presence of a malignant process.
In addition to melanoma, an increase in Beta-2-microglobulin in the urine is observed with:
- diabetic kidney damage;
- side effects of nifedipine, gentamicin and other drugs;
- autoimmune diseases, such as systemic lupus erythematosus.
In the blood, an increase in Beta-2-microglobulin in the blood is observed when:
- acute total inflammation;
- autoimmune processes;
- severe viral infections - HIV, CMV, etc.;
- renal failure;
- multiple melanomas.
Based on the interpretation of the results of tests for Beta-2-microglobulin, it is possible to assume the development of skin cancer with concomitant clinical manifestations and enlargement of regional lymph nodes.
The amount of S100 protein in the blood of a healthy adult should not exceed 0.105 μg/l. An increase in this tumor marker indicates:
- the presence of a malignant process on the skin, that is, confirms melanoma;
- neurological disorders (stroke, brain injury, Alzheimer's disease, cerebral vascular sclerosis, etc.);
- intense physical activity the day before.
As the tumor process spreads, the results of the S100 protein analysis will increase in direct proportion.
The reasons for re-analysis may be the identification of early relapses in preclinical manifestations. When tumor cells infect the lymph nodes and spread through the lymph system to other subcutaneous layers, but do not appear on the surface of the body, the S100 protein begins to increase.
With metastases to other organs, the corresponding substances begin to be produced. When healthy cells die and cancer cells grow, lactate dehydrogenase (LDH), tumor necrosis factor (TNF) and other markers increase.
SCCA
It is also a protein compound synthesized by flat epithelial cells of the skin and mucous membrane. When performing diagnostic manipulations, the same problems arise as when analyzing the S-100 tumor marker.
An increase in SCCA concentration is observed only in 44% of cases with diagnosed melanoma. In the blood of a healthy person, this value is no more than 2 nanograms per milliliter.
By examining the protein volume of squamous cell carcinoma, the growth and spread of the malignancy can be monitored.
What affects the accuracy of the analysis
Some medications, when broken down, release substances that affect the level of tumor markers in the blood. There may be similarities in chemical composition, so laboratory analyzers mistake these substances for the chemical composition of tumor markers and may give a false positive answer. Other medications activate the production of markers in healthy tissues.
Before taking tumor markers for skin melanoma, you should consult your doctor about the medications you are taking. It is advisable to stop taking carboplatin, cisplatin, etc.
There are no exact markers for the specificity of the oncological process. The production of specific proteins is influenced by the functioning of the immune and humoral systems. In a number of patients, when there are failures in these systems, an increase in tumor markers is not detected, even with stage 2-3 skin cancer.
Research quality
Once again, it is worth emphasizing that skin cancer is one of the most difficult types of oncology in terms of diagnosis. Its early stage is almost imperceptible and asymptomatic. The levels of tumor markers in the body may be slightly elevated, but the disease has already begun its destructive effect. The increase in protein in the body can also be affected by colds, infections, cysts, benign formations and some other factors.
Research at the DNA level has proven to be the best in detecting melanomas. However, even here difficulties may arise. This study is based on comparing tests before and during illness, but doctors don't always have patient material to compare with. Not every person gives their DNA, suspecting that they will someday be diagnosed with cancer.
The S100 tumor marker is widely used not for diagnosis, but during treatment. Its level in the blood directly depends on the size of the malignant neoplasm and the spread of metastases. After surgery or an intensive course of treatment, the S100 level should decrease and if it starts to increase again, then either the tumor has begun to grow again or metastases have gone undetected. Based on this, the oncologist can draw the necessary conclusions and prescribe more correct and high-quality treatment.
And yet, despite the danger of skin cancer, you should not immediately fall into despair. Medicine and science do not stand still, which means that every day diagnostic and treatment methods are improved, new methods are found and explored that will give hope even when everything has been tried.
Modern tendencies
The question of more frequent use of tumor markers in diagnosis is being raised in medicine. But this requires a whole range of additional measures. It should be taken into account that a number of malignant neoplasms still remain poorly studied. There are difficulties in this type of research, which are associated with the inability to conduct tests on sick people. At least, this possibility is not always available.
In the early stages, melanoma is diagnosed using RNA and DNA tests. For this purpose, the patient also donates blood. Sick and healthy samples are compared. As a rule, the source of cancer is genetic defects. And if this is detected in the early stages, the presence of malignant neoplasms is assumed before the tumor markers appear. DNA diagnostics is still being studied and continues to be improved. However, there are already first successes: changes in gene activity are being recorded in certain types of malignant neoplasms.
Thus, when understanding the issues of tumor markers for melanoma, you need to take into account that there is not one that can 100% determine the presence of cancer in the body. And even if their concentration is increased, this does not mean that the person is suffering from cancer. In any case, a doctor’s consultation, diagnosis, treatment are necessary - all this is carried out taking into account the individual characteristics of the patient and circumstances.
Stages of development
The stage of development is determined according to the accepted international classifier. Diagnosis of melanoma occurs by determining its thickness and modifications according to the following criteria:
- Stage zero is early. A small thin spot that does not disturb the surface layer.
- The first is a slight increase in thickness.
- Second, the tumor reaches medium size.
- Third, adjacent tissues and lymph nodes are affected by diseased cells.
- Fourth – metastases begin in distant organs and tissues.