Pyoderma is a group of purulent-inflammatory skin diseases that develop as a result of the activity of pathogenic microorganisms. Most often, the development of pathologies is promoted by staphylococci, streptococci, Proteus vulgaris and Pseudomonas aeruginosa. Approximately a third of all dermatological diseases are primary or secondary pyoderma. The first ones occur with primary damage to the skin. The latter are a complication that occurs when scratching the skin (an infection gets into the wound). Pyoderma can develop against the background of scabies, eczema, chronic renal failure and even diabetes. A dermatologist diagnoses and treats the disease. In therapy, it is important to sanitize pathological foci, as well as treat concomitant somatic diseases.
…
What is pyoderma?
Pyoderma is a group of pustular dermatoses that develop as a result of purulent inflammation of the skin, subcutaneous fatty tissue and skin appendages.
This skin disease (pyoderma) can occur as a result of skin infection by various microorganisms, but the main causes of the disease are staphylococci and streptococci.
A predisposing factor contributing to the frequent occurrence of pyoderma is the fact that the skin is an open biological system, abundantly colonized by opportunistic microorganisms.
The skin can be colonized by white and epidermal staphylococci, Staphylococcus aureus (in about forty percent of people), various corynebacteria, Malassezia furfur, etc.
The degree of skin contamination with various microorganisms, as well as the composition of the skin microflora varies significantly and depends on individual characteristics (age, hormonal levels of the patient, adherence to personal hygiene rules, climatic conditions, living conditions, state of the immune system, etc.).
Microorganisms enter:
- exogenous (from the external environment);
- endogenous (the presence of foci of chronic infection, colonization by staphylococci and other microorganisms of the mucous membranes of the nasal cavity and pharynx, etc.);
- due to the active reproduction of opportunistic microorganisms already living on the skin and mucous membranes.
It should be noted that the quantitative and qualitative components of the skin microflora are dynamic, that is, they are constantly changing. This is due to constant exposure of the skin to environmental factors (dust, air, water, etc.).
Normally, the skin is most often contaminated with white and epidermal staphylococci. The greatest accumulation of these microorganisms is observed in the area of skin folds, under the nails, as well as on the mucous membranes of the nasal cavity and pharynx.
Staphylococcus aureus most often inoculates the mucous membranes of the nasal cavity (especially the wings of the nose), the skin of the armpits, and the perineum. Approximately forty percent of people are permanent carriers of Staphylococcus aureus on the skin and mucous membranes.
Complications
Severe consequences of pustular diseases are observed with:
- untimely access to a medical institution;
- weak immunity;
- undergoing an incomplete course of therapy;
- use of questionable treatment methods;
- poor hygiene;
- preservation of provoking factors.
Complications:
- inflammation of the lymph nodes;
- abscesses;
- scars in areas of self-removal of pustules; infection of bone tissue;
- blood poisoning;
- thrombosis of cerebral vessels;
- meningitis;
- inflammation of internal organs.
[adsen]
What causes pyoderma?
The causes of pyoderma development are pathogenic or conditionally pathogenic microorganisms that abundantly colonize the skin. Most often, the cause of the development of pyoderma are staphylococci, streptococci, Pseudomonas aeruginosa, various fungi, pneumococci, Escherichia coli. Less commonly, the inflammatory process in the skin and subcutaneous fat can be caused by the association of various pathogenic microorganisms (pseudomonas and Escherichia coli, bacteroides and enterococci, etc.).
Pyoderma in newborns (epidemic pemphigus of newborns) is caused by Staphylococcus aureus.
Is pyoderma contagious or not?
A highly contagious type of pyoderma is considered to be epidemic pemphigus of newborns, caused by Staphylococcus aureus and erysipelas (streptococcal inflammation).
A patient with pustular skin lesions can serve as a source of these bacteria. In most cases, a child becomes infected from a mother who has an active purulent inflammatory process (furuncle, hidradenitis, etc.). Less commonly, infection can occur from a healthy carrier of staphylococci.
Most pyodermas are caused by saprophytic microorganisms and are not contagious. That is, in the presence of associated risk factors (stress, endocrine pathologies, injuries, decreased immunity, etc.), skin inflammation can develop due to opportunistic microorganisms that constantly colonize the skin.
Despite the fact that the same Staphylococcus aureus can be found in most people and is not accompanied by the development of an inflammatory process, in the presence of risk factors they can cause severe pyoderma.
Menu (Power Mode)
Alternating different protein and cereal dishes throughout the week will make the menu varied. Remember that fish dishes should prevail over meat dishes, and vegetables or fruits should be included at every meal. Enrich your dishes with bran and, if you are allowed, with various seeds and seeds; use cold-pressed vegetable oils in salads, constantly alternating them. Use fruits and low-fat yogurt for snacks. With your doctor's permission, fermented milk products should be included in your diet daily.
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
How is pyoderma transmitted?
Staphylococci, streptococci, pneumococci, etc. can enter the body and skin through airborne droplets or contact (household or personal hygiene items). Autoinfection (infection from a distant focus on the patient’s body) is also possible.
Predisposing factors contributing to the development of pyoderma
For the development of an inflammatory process in the skin and subcutaneous fat, the mere fact of pathogenic microorganisms entering the skin (provided there is no damage to it) is not enough. In the absence of favorable factors, the activity of pathogenic and opportunistic microorganisms is completely suppressed by local immune factors.
Predisposing factors that contribute to the occurrence of inflammation in the skin and subcutaneous fat tissue are:
- the presence of violations of the integrity of the skin and mucous membranes (wounds, abrasions, burns, frostbite, bedsores, etc.);
- microcirculation disorders in tissues (thrombosis of the veins of the lower extremities, diabetes mellitus, etc.);
- long-term treatment with glucocorticosteroids and immunosuppressants;
- increase in skin pH;
- the presence of hypovitaminosis or vitamin deficiency;
- endocrine pathologies (diabetes mellitus, polycystic ovary syndrome, etc.);
- changes in hormonal levels, accompanied by changes in the composition of sebum or an increase in its production;
- the presence of functional pathologies of the central nervous system;
- various immunodeficiencies;
- excessive dry skin;
- exhaustion, prolonged sleep deficit, overwork, frequent stress;
- violation of personal hygiene rules;
- improperly selected skin care;
- use of cosmetics with aggressive ingredients;
- mechanical or chemical irritation of the skin;
- excessive consumption of easily digestible carbohydrates;
- deficiency of various microelements (most often zinc deficiency);
- presence of obesity;
- the presence of foci of chronic infection;
- alcohol abuse;
- the presence of dermatitis, psoriasis, etc.
Disease prevention
Preventive measures against various types of pyoderma are simple and easy to perform. These include:
- mandatory and early antimicrobial treatment of small wounds and skin abrasions;
- maintaining cleanliness of the skin and taking measures against its excessive contamination during work, including home gardens;
- treatment of any foci of inflammation and chronic infection, including the nasopharynx and foci of caries;
- early contact with a doctor at the first signs of skin changes and timely diagnosis.
Classification of pyoderma
Depending on the main causative agent of the inflammatory process, pyoderma is usually divided into staphylococcal, streptococcal, mixed (streptostaphyloderma).
According to the duration of its course, inflammation is divided into acute and chronic.
Depending on the depth of the lesion, pyoderma can be superficial or deep.
According to the mechanism of occurrence, pyoderma can be primary or secondary (develops as a complication of various dermatoses - scabies, psoriasis, eczema, atopic dermatitis, herpes, traumatic lesions of the skin, etc.).
Read further: Photos, symptoms and treatment of psoriasis in adults and children, causes of the disease
Also, when determining the type of pyoderma, one should take into account the prevalence of skin lesions (limited or diffuse inflammation), the localization of inflammation, the involvement of hair follicles, sweat glands, skin folds, periungual ridges, etc. in the inflammatory process.
The most convenient is the separate classification of staphyloderma and streptoderma.
- Staphylodermic pyoderma in children and adults can be:
- Superficial: - ostiofolliculitis; - folliculitis; - sycosis; - vesiculopustulosis; — epidemic pemphigus of newborns (the most severe pyoderma in children); -exfoliative dermatitis (Ritter's disease); - staphylococcal scalded skin syndromes; - staphylococcal toxic shock syndromes;
- Deep - boils; - furunculosis; - carbuncles; - abscesses; - pseudofurunculosis; - hidradenitis.
Read further: Choosing the most effective antibiotics for furunculosis in tablets and creams
- Streptoderma:
- Superficial - streptococcal impetigo; - crevice impetigo; - paronychia; - papulo-erosive streptoderma; — intertriginous streptoderma; - erysipelas; — streptococcal toxic shock syndromes; — acute diffuse streptoderma.
- Deep: - cellulite; - ecthyma vulgar.
Read further: 7 groups of antibiotics for erysipelas of the leg or arm
- Streptostaphyloderma:
-superficial vulgar impetigo;
- chancriform pyoderma.
Gangrenous pyoderma, which is a chronic neutrophilic progressive necrosis of the skin, is included in a separate subclass. The exact etiology of the disease is unknown. As a rule, pyoderma gangrenosum is associated with various autoimmune diseases.
Gangrenous pyoderma photo
Pyoderma - photos, treatment and symptoms
All pyoderma differ significantly in symptoms, prognosis and treatment. The clinical picture depends on the pathogen, localization and severity of inflammation, etc.
Ostiofolliculitis
With the development of ostiofolliculitis (Bockhard's impetigo), the appearance of pointed, small, yellowish-white pustules with a hair in the center is noted. In this case, the inflammatory process develops at the mouth of the hair follicles.
A characteristic halo of hyperemia (redness) forms around the purulent pustule. This type of pyoderma most often develops in men in the area of the beard or mustache (pyoderma on the face is quite common). This pyoderma is rare on the skin of the body and around vellus hair.
This pyoderma practically does not occur in children before puberty.
Spontaneous opening of the pustule is usually observed by the third or fourth day. There are no scars left.
Folliculitis
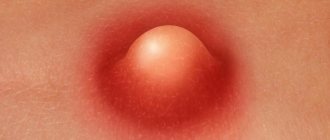
Folliculitis is characterized by the development of acute inflammatory damage to the hair follicles. In this case, a red, dense, painful infiltrate appears around the inflamed follicle. Over the course of several days, a pustule forms in the center.
After five to seven days, the pustule gradually dries out with the formation of yellowish crusts.
In some cases, purulent melting of the inflammatory infiltrate with the appearance of a scar is possible.
Staphylococcal pyoderma: photo of facial skin lesions
Vesiculopustulosis
With this type of pyoderma, a purulent-inflammatory process affects the mouths of the merocrine sweat glands. This pyoderma is registered more often in children than in adults. In most cases, the development of this pyoderma in children is preceded by prickly heat.
The rashes are initially single, small, bright red. Subsequently, the formation of a pustule is observed in the center of inflammation. Most often, the rash is localized on the torso, scalp and skin folds.
In children with immunodeficiency conditions, without timely medical care, the inflammatory process can quickly spread, leading to the occurrence of abscesses and phlegmon. In severe cases, the disease may be complicated by sepsis.
Photos of pyoderma in children
Epidemic pemphigus (pyococcal pemphigoid) of newborns
The disease is highly contagious (contagious).
Symptoms of this pyoderma in children develop within 3-10 days after birth. The appearance of flaccid blisters (phlyctena) of various sizes on the skin is noted. The contents of the conflict are cloudy, the formations themselves are surrounded by a halo of inflammatory redness.
Subsequently, the contents of the conflict quickly fester. The flicten tire is very thin and breaks easily, leading to the appearance of erosive surfaces. Crust formation is not typical.
The period of rash can last from several days to several weeks.
An increase in temperature, lethargy, tearfulness of the child, refusal to eat, etc. are also noted.
Pyoderma in newborns - photo of the skin
Authorized Products
- Bran bread, whole grain bread, bran bread and oatmeal cookies.
- It is advisable to cook soups in vegetable broth with the addition of cereals and vegetables. It is better to exclude meat and fish broths or use secondary broth.
- Second courses are prepared from veal, beef, chicken or turkey (meat is selected according to individual tolerance and with the permission of a doctor in each specific case). They are prepared in pieces, boiled or baked. Minced meat products are also baked with low-fat sauce (sour cream or tomato with a doctor’s permission).
- Any fish is allowed (dietary and fatty - mackerel, cod, salmon, herring). Avoid if you are intolerant to fish protein. It can be stewed, boiled, baked. The daily presence of fish in the diet is desirable, since its protein is easier to digest and has less load on the kidneys and liver.
- Any vegetables (according to preference and tolerance) up to 600 g per day. In special cases, some vegetables are excluded or limited. Half of the vegetables should be consumed raw, since their nutritional and vitamin value is greater than that of heat-treated ones. Avoid out-of-season greenhouse vegetables grown using mineral fertilizers.
- Include in the menu daily fruits allowed for each skin disease (up to 500 g). They are rich in dietary fiber and vitamins. Preference should be given to fruits that are seasonal and grown in the area.
- Additionally, consume foods high in dietary fiber that remove toxins: bran, prunes, gooseberries, raspberries, dates, cranberries, figs, raisins and dried apricots.
- Chicken and quail eggs, boiled or in the form of an omelet. They are excluded if you are allergic to chicken protein.
- Low-fat dairy products. Mild cheeses, cottage cheese. Give preference to natural kefir and yogurt with bifidobacteria . Dairy products should not contain dyes or preservatives. In this regard, it is better to prepare your own yoghurts and kefir from pharmacy starters.
- All cereals are allowed. You can make casseroles and cereals with cottage cheese. Preference should be given to whole grains rather than processed cereals and instant cereals with sugar, preservatives and flavor substitutes.
- Pasta products are allowed from durum wheat. Excluded if you are overweight.
- Include a variety of vegetable oils as a source of healthy polyunsaturated fatty acids.
- Sauces can be prepared using low-fat sour cream, fruit or vegetable oils.
- Drinks include weak tea with milk, green tea, herbal infusions (if you are not allergic to herbs), compotes, any juices, rosehip infusion.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cabbage | 1,8 | 0,1 | 4,7 | 27 |
| Brussels sprouts | 4,8 | 0,0 | 8,0 | 43 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| potato | 2,0 | 0,4 | 18,1 | 80 |
| cucumbers | 0,8 | 0,1 | 2,8 | 15 |
| salad pepper | 1,3 | 0,0 | 5,3 | 27 |
| salad | 1,2 | 0,3 | 1,3 | 12 |
| soybeans | 34,9 | 17,3 | 17,3 | 381 |
| soybeans (sprouts) | 13,1 | 6,7 | 9,6 | 141 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
Fruits | ||||
| watermelon | 0,6 | 0,1 | 5,8 | 25 |
| pears | 0,4 | 0,3 | 10,9 | 42 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Nuts and dried fruits | ||||
| raisin | 2,9 | 0,6 | 66,0 | 264 |
| dried apricots | 5,2 | 0,3 | 51,0 | 215 |
| prunes | 2,3 | 0,7 | 57,5 | 231 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| cereals | 11,9 | 7,2 | 69,3 | 366 |
| Wheat groats | 11,5 | 1,3 | 62,0 | 316 |
| brown rice | 7,4 | 1,8 | 72,9 | 337 |
Raw materials and seasonings | ||||
| milk sauce | 2,0 | 7,1 | 5,2 | 84 |
| sour cream sauce | 1,9 | 5,7 | 5,2 | 78 |
Dairy | ||||
| kefir | 3,4 | 2,0 | 4,7 | 51 |
| sour cream | 2,8 | 20,0 | 3,2 | 206 |
| curdled milk | 2,9 | 2,5 | 4,1 | 53 |
Cheeses and cottage cheese | ||||
| cottage cheese | 17,2 | 5,0 | 1,8 | 121 |
Meat products | ||||
| beef | 18,9 | 19,4 | 0,0 | 187 |
| veal | 19,7 | 1,2 | 0,0 | 90 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| chicken | 16,0 | 14,0 | 0,0 | 190 |
| turkey | 19,2 | 0,7 | 0,0 | 84 |
Oils and fats | ||||
| peasant unsalted butter | 1,0 | 72,5 | 1,4 | 662 |
| wheat germ oil | 0,0 | 100,0 | 0,0 | 884 |
| linseed oil | 0,0 | 99,8 | 0,0 | 898 |
| olive oil | 0,0 | 99,8 | 0,0 | 898 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
| green tea | 0,0 | 0,0 | 0,0 | — |
Juices and compotes | ||||
| juice | 0,3 | 0,1 | 9,2 | 40 |
| jelly | 0,2 | 0,0 | 16,7 | 68 |
| rose hip juice | 0,1 | 0,0 | 17,6 | 70 |
| * data is per 100 g of product | ||||
Treatment of pyoderma at home
All treatment must be prescribed by a dermatologist. Most pyoderma (folliculitis, sycosis, etc.) does not require hospitalization and treatment can be carried out at home.
Treatment of pyoderma in adults
The goal of treatment is to accelerate the resolution of purulent inflammation, accelerate the regeneration of the epithelium and reduce the frequency of relapses of inflammation.
The main drugs prescribed for pyoderma are antibiotics (local or systemic). According to indications, local or systemic retinoids may be prescribed.
In isolated cases, in severe cases (chronic ulcerative forms, gangrenous, etc.), systemic administration of glucocorticosteroids may be required.
In frequently relapsing forms of the disease, immunomodulatory and immunostimulating therapy may be required.
Antiseptic solutions, zinc preparations, salicylic acid, antibacterial ointments or lotions can be used for external skin treatment.
Hormonal ointments can be used strictly according to indications.
For systemic antibacterial therapy, doxycycline, azithromycin, cephalexin, cefazolin, ciprofloxacin, etc. can be used. The choice of antibiotic depends on the severity of the patient's condition.
In severe recurrent cases, retinoid drugs may be prescribed.
For deep variants of pyoderma, UHF therapy is used
Diagnostics
To determine the most effective treatment method for pyodermatitis, correct diagnosis is very important. It includes the following procedures:
- History according to the patient.
- Visual examination by a dermatologist.
- Laboratory microbiological and immunological tests, including examination of pus, general blood test, urine test and others.
- Differential diagnosis, the purpose of which is to exclude diseases with similar symptoms (syphilis, vasculitis, tuberculosis).
In some cases, to clarify the diagnosis, it may be necessary to consult other specialists - a therapist, a neurologist, an allergist, an endocrinologist . Pregnant women require observation by a gynecologist, and children - a pediatrician.