Scleroderma is a diffuse disease of connective tissues that appears due to increased compaction of organs and reduced blood supply. Scleroderma can affect the gastrointestinal tract, heart, lungs, kidneys and liver. Most often, this disease affects females. The skin of patients hardens, which indicates damage to small vessels. The causes of the disease are unknown to this day. However, some scientists argue that congenital inferiority of the immune system is to blame. There is no exact confirmation of this theory.
ethnoscience
Of course, traditional medicine has already developed many recipes for remedies that help in the treatment of scleroderma. But self-medication should only be done using proven methods and only after examination by a specialist. Basically, the currently known traditional medicine serves only as an addition to the main, professional treatment. Such means include:
- compress when using aloe juice
- a solution of dry wormwood, wormwood juice and petroleum jelly, mixed with pig fat in a ratio of one to five, also for a compress
- ointment containing tarragon diluted with nutria fat, also in a ratio of one to five
- decoctions of St. John's wort and other medicinal plants for internal use
In order to mix tarragon ointment with nutria fat, the fat must be melted in a water bath, and to mix the entire composition must be simmered at a low temperature of about 35-40 degrees for 6 hours.
Folk remedies
Doctors do not recommend treating scleroderma with folk remedies. The mechanism of the pathology is too subtle, there is a lot of unknown in the prognosis. It is impossible to foresee the benefits or harm from herbal decoction or other procedures in advance. The obsession with kefir lotions when hormonal therapy is indicated is regrettable.
Traditional medicines describe the following methods:
- applying ichthyol ointment or a tampon with aloe juice to the skin after steaming in a bath;
- compresses made from baked onion and honey;
- ingestion of a decoction of knotweed, lungwort and horsetail;
- a decoction of bearberry and lingonberry leaf to detect kidney damage;
- disinfection of ulcers on the fingers with baths of oak bark and nettle leaves.
Reviews of treatment methods vary, since the forms of the disease and the expected response of each organism are individual. Any treatment must be agreed with a doctor. Be aware of the possibility of unusual drug reactions. Patients should not add to their suffering through experiments.
Scleroderma - what is this disease?
The disease in question is an autoimmune damage to any connective tissue and blood vessels against the background of both inflammation and generalized fibrosis and disturbances in the microcirculation of biological fluids. The term “scleroderma” can be explained more simply by what this lesion is:
- skin;
- structures of the musculoskeletal system;
- kidney;
- hearts;
- digestive tract organs;
- liver.
Scleroderma - pathogenesis
To develop effective therapy and search for new medications for this pathology, it is important to understand the mechanisms of its development. Since the 40s of the last century, scleroderma has been studied, what it is and how to treat the disease.
The causes or factors provoking the problem have not yet been precisely established, but the mechanisms of its progression have been thoroughly determined.
A key role in the pathogenesis of the disease belongs to humoral and cellular immunity. Disturbances in their work lead to an increase in the concentration of CD4+ and B lymphocytes. A hypersensitivity reaction occurs, and a huge number of autoantibodies and circulating protective complexes of various types are formed. Fibroblasts become hyperactive and attack both the connective tissues and blood vessels of the body.
Excessive production and accumulation of collagen begins. This simultaneously provokes acute inflammatory processes, which quickly develop into a chronic form, which is difficult to treat. Because of these features, the definition of what scleroderma is includes the word “autoimmune.” The cells of the defense system perceive their own organic structures as foreign and destroy them.
Scleroderma - causes
The exact factors causing changes in immune function are not yet known. The knowledge gained through medical research helps to determine only the mechanisms due to which scleroderma occurs, what it is, and how to treat the pathology. There are several theories of the origin of the described disease and individual etiological hypotheses. Scleroderma may have the following causes:
- genetic predisposition;
- cytomegalovirus infection;
- streptococcal sore throat;
- complications of influenza;
- prolonged exposure to chemicals;
- taking medications such as cytostatics;
- stress;
- hypothermia and frostbite;
- mechanical injuries of the body;
- exposure to vibration;
- hormonal changes;
- improper vaccination;
- surgical interventions, including operations in the oral cavity (tooth extraction, tonsil removal).
Scleroderma - treatment
There are no methods yet that provide complete relief from the described disease. You can only slow down its progression and mitigate the negative manifestations that systemic scleroderma causes; treatment is predominantly symptomatic. Its effectiveness depends on the stage, form and severity of the disease, and the person’s readiness to change his lifestyle.
Scleroderma - clinical guidelines
The main therapy for the pathology is carried out by a rheumatologist. In accordance with the organs that have undergone changes, other specialists who know what is characteristic of scleroderma, what it is, and how to effectively treat the disease can be involved:
- dermatologists;
- cardiologists;
- nephrologists;
- gastroenterologists;
- pulmonologists;
- endocrinologists;
- psycho- and physiotherapists.
Together, doctors develop a comprehensive individual plan, including drug treatment and general measures.
Systemic scleroderma - clinical recommendations:
- Quitting smoking and caffeine consumption.
- Maintaining physical activity.
- Controlling body temperature (avoiding cold).
- Gentle skin care.
Medicines for scleroderma
Due to the variety of symptoms, systemic medications are selected from several pharmacological groups:
- vasodilators (Nifedipine, Diltiazem);
- anticoagulants (Warfarin, Heparin);
- phosphodiesterase inhibitors (Sildenafil);
- prostanoids (Iloprost);
- antiplatelet agents (Pentoxifylline, Aspirin);
- endothelin receptor blockers (Bosentan);
- anti-inflammatory drugs (Nimesulide, Diclofenac);
- antibiotics (Ciprofloxacin, Sumamed);
- glucocorticoids (Prednisolone, Methylprednisolone);
- immunosuppressants (Cyclosporine, Azathioprine) and others.
Additional medications (heart, kidney, pulmonary, digestive) are prescribed depending on the affected organs. Local medications are used to relieve dermatological signs. Ointment for scleroderma is selected with corticosteroid components:
- Sinaflan;
- Hydrocortisone;
- Elokom-S;
- Akriderm SK;
- Betaderm and analogues.
Physiotherapy for scleroderma
Non-drug treatment methods help relieve the symptoms of the pathology. Certain forms of the disease, such as linear and plaque scleroderma, are greatly improved through physical therapy. Effective methods of influence:
- ultraphonophoresis;
- vacuum decompression;
- magnetic therapy;
- radon, nitrogen, hydrogen sulfide baths;
- electrophoresis
- decimeter wave therapy;
- ozokerite applications;
- massage;
- laser therapy;
- applying mud;
- hyperbaric oxygen therapy;
- aerocryotherapy and others.
Scleroderma - traditional methods of treatment
Alternative medicine is not approved by rheumatologists and its use is extremely rare. Local remedies can still help if limited scleroderma is diagnosed; in the systemic form of the disease they are ineffective. Among external folk remedies, a fat-based ointment is often used. It relieves irritation and softens rough skin, moisturizes it.
Ointment recipe for scleroderma
Ingredients:
- wormwood herb – 100 g;
- lard – 0.5 kg.
Preparation, use
- Melt the pork fat in a steam bath.
- Mix it with well-chopped wormwood.
- Place the mixture in the oven for 6 hours at temperatures up to 150 degrees.
- Strain the product and pour into a clean jar.
- Cool the ointment in the refrigerator.
- Apply the medicine to the affected areas three times a day.
- Continue treatment for 3 months.
Diet for scleroderma
A special diet is not being developed as part of complex therapy for pathology. Meals for scleroderma should be frequent and divided, healthy, complete and balanced. Some foods on the menu just need to be limited or excluded:
- fatty foods;
- smoked meats;
- fried food;
- canned food;
- hot spices;
- alcohol.
Causes of the disease
The causes of this disease are not fully understood. It is assumed that the development of pathology is influenced by genetic factors. There is a hereditary predisposition to autoimmune diseases. This does not mean that the disease will appear immediately after birth; the pathology can develop at any age.
In people with a tendency to scleroderma, the following factors can trigger the onset of the disease:
- past infections;
- hormonal disorders;
- hypothermia (especially frostbite on the hands and feet);
- molecular mimicry of microorganisms, which results in increased activity of lymphocytes;
- hormonal disorders;
- intoxication with drugs or chemicals;
- poor ecology of the place of residence;
- work associated with harmful effects (for example, in chemical production).
The environment and human health are closely interconnected. Very often, the development of scleroderma is provoked by living in a region with a large number of industrial enterprises. This is especially true for the juvenile form of the disease, which manifests itself at an early age. Silicon dioxide, white spirit, welding gases, ketones, solvents, trichlorethylene can have a harmful effect. Not every person whose work involves these substances will necessarily develop the disease. But with a hereditary predisposition, the risk of scleroderma due to constant contact with chemical compounds is very high.
Prevention of scleroderma
It’s not that difficult to protect yourself from hardening of the skin. The main thing is to follow a few simple rules:
- avoid hypothermia of the body, insulate well in the cold season;
- wear loose shoes;
- Avoid prolonged exposure to air conditioning in hot weather;
- drink less coffee, since caffeine causes spasms and constriction of peripheral blood vessels, which contributes to the development of scleroderma.
If scleroderma is detected in one of the family members, all relatives should be tested, since there are often cases when the disease spreads within the family.
Mechanism of development of OSD
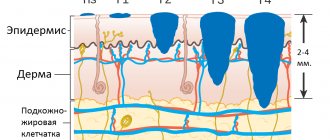
Localized scleroderma is based on impaired circulation in the capillaries, changes in the metabolism of fibroblasts, dysfunction of endothelial cellular structures, increased deposition of collagen, which is responsible for the elasticity of the epidermis, in the skin against the background of immune
Negative factors of different nature and strength of influence activate autoimmune processes in the body. Immune cells mistake their own epidermal structures for “enemies,” foreign agents. The production of collagen, a connective tissue protein, increases.
Against this background, vascular changes occur, the inner wall thickens, and blood flow is disrupted. Blood viscosity increases, which leads to stagnation and inflammatory processes.
How to treat scleroderma at home? Folk recipes
I won’t hide it, systemic scleroderma is a serious disease, and recovery is difficult: it should be carried out with the active participation of the patient and his relatives.
For treatment, available medicinal plants are used, used in the form of decoctions, infusions, tinctures, juices, ointments, inhalations, and applications.
Sources of natural silicon used for all dermatitis, problems with cartilage, bone, and connective tissue are horsetail, knotweed, dandelion, birch leaves and buds.
Among the plants that improve blood flow, sweet clover, horse chestnut, and stinging nettle are effective; anti-inflammatory drugs - calendula officinalis flowers, barberry root, raspberry leaf, blackberry leaf, birch leaf, walnut leaf; natural regenerators - plantain, licorice root; immunity correctors include duckweed, wheatgrass roots, and burdock.
For localized scleroderma
When only the skin is affected, a medicinal mixture has worked well, in which all the plants, dried and crushed, are taken in equal proportions, for example, 30-50 grams. These are licorice root, wheatgrass, string grass, sage, duckweed, calendula flowers, black elderberry, meadowsweet, nettle leaf, birch, currant.
Take 1 tbsp. spoon of the mixture, pour 0.5 liters of water, bring to a boil, keep on low heat for 5-7 minutes. Leave for 1 hour, then, after straining, add 1 tbsp to the broth. a spoonful of honey and 1 tbsp. a spoonful of juice (plantain, elderberry, burdock, to choose from). Take 70-100 ml before or after meals 3-4 times a day. Heal until the entire collection is over.
Externally, use calendula ointment (sold at the pharmacy) - apply a thin layer to the affected areas of the skin 2 times a day. You can prepare such an ointment with an anti-inflammatory effect yourself by mixing dried, powdered calendula flowers with baby cream or castor oil in a ratio of 1:3 or 1:5.
But what plants will help with systemic scleroderma
If pulmonary lesions are observed, the collection will include plantain, lungwort, licorice root, wheatgrass, marshmallow, elecampane, linden flowers, calendula, duckweed, thyme, string. All dried, crushed components of the collection are also taken in equal parts, 30-50 g each, and the decoction is prepared according to the same scheme as for the localized form.
The only difference is that in addition to burdock and plantain juices, you can add thyme and elderberry juices to the broth, also to choose from.
For joint lesions, we give preference to the roots of burdock, rose hips, cinquefoil, licorice, wheatgrass, and water lilies; birch, raspberry, currant leaves; poplar buds. The cooking method is the same as in previous recipes. Of the juices that come as an additional component, I can recommend the juices of burdock, birch, and rowan.
Lichen sclerosus - white spot disease
It is more common in women after 50 years of age, mainly due to hormonal disorders, as well as in children from one to 13 years of age (70% of cases under 7 years of age).
The spotted superficial variant of focal scleroderma is characterized by the formation of small spots ranging in size from 0.5 to 1 cm, snow-white, pearlescent in color, with thin, shiny, transparent skin, surrounded by a narrow erythematous corolla, reminiscent of the lilac ring in plaque scleroderma.
The favorite localization of this form of scleroderma is the skin of the neck, chest, shoulders, genitals, and less often on the back and abdomen.
There is no hair in the area of the spots, the skin pattern is smoothed. The spots are often grouped, forming extensive lesions with a diameter of up to 10 cm or more. Subjectively, a feeling of skin tightness and slight itching may be disturbing.
The second most common localization of lichen sclerosus is in the perivulvar or perianal zone in the form of an “eight” or “hourglass”, the foreskin and the glans penis.
In adults, rashes persist for a long time, leaving behind atrophy.
When lichen sclerosus occurs in children in the genital area, the prognosis is favorable. Symptoms of the disease disappear within a period of one to ten years, in 60-70% of cases by puberty the condition of patients improves significantly. In rare cases, the disease persists into adulthood. Long-standing lesions may be sensitive, especially when walking. There may be some complications associated with impaired urination and pinching of the glans penis.
Classification
Scleroderma is divided into two subtypes:
- Systemic. With this type of pathology, not only tissue located in the skin structures is involved in the autoimmune process, but also tissue that is part of the internal organs.
- Focal. The pathological process involves the skin; in some cases, the disease affects nearby structures: cartilage, muscles, bones. It occurs more often and responds better to treatment.
There is a separate subtype of systemic scleroderma that occurs in children under the age of sixteen: juvenile scleroderma. This type of pathology is often detected in preschool age.
Subtypes of focal scleroderma, depending on the characteristics of skin manifestations:
- linear;
- plaque;
- teardrop-shaped.
Read about how to treat impetigo on the skin of children here.
Linear scleroderma
The linear form of scleroderma is less common; in 48% it occurs in childhood (infantile scleroderma), mainly in girls. It is an unfavorable variant of the course, because it often develops into systemic scleroderma.
Linear scleroderma can develop in the first and second decades of life, while the typical variant of limited scleroderma in a localized or generalized form is observed mainly in adults.
The lesion usually develops first on the scalp,
then spreads to the skin of the forehead,
the bridge of the nose, resembling the scar after a blow with a saber (coup de sabre).
When the subcutaneous tissue, muscles and sometimes bone are affected, this form of linear scleroderma is defined as facial hemiatrophy or Parry-Romberg syndrome.
Lesions in the form of stripes can also be located on the limbs.
The course of linear scleroderma is the same as plaque scleroderma: first swelling develops, then hardening, and the process ends with atrophy.
Complaints and anamnesis in adults and children
- Itchy skin (common complaint).
- Difficulty swallowing solid foods. May be accompanied by difficulty swallowing liquids and subsequent nausea, vomiting, weight loss, abdominal cramps, wet diarrhea and fecal incontinence.
- The patient may experience shortness of breath during exercise and at rest.
- Rapid heartbeat without characteristic chest pain, fatigue and shortness of breath.
- Joint pain, limited movement, joint swelling and muscle pain.
REFERENCE! Systemic sclerosis first manifests itself as joint pain in 15%. As inflammatory myopathy – in 10% of patients. Weakness and general malaise – in 80% of patients.
Symmetrical swelling of the fingers and hands appears, which is generalized to involve the forearms, face, trunk and lower extremities. Over time, the swelling develops into hard, associated induration and fibrosis, which eventually causes deformation of the fingers.
Complaints in children include
- loss of skin's ability to stretch;
- reduced hand functionality;
- severe sensitivity to cold;
- enlarged blood vessels on the hands, face, and around the nail beds;
- subcutaneous calcium deposits (calcinosis).
The history of the disease and the study of the patient’s complaints are closely intertwined with the history of the development of scleroderma.
The medical history will consist of both personal and family medical history.
The anamnesis (in addition to biographical information) includes information about:
- bad habits;
- first manifestation of the disease;
- severity of symptoms;
- hereditary pathologies causing systemic sclerosis;
- provoking factors (stress, acute and chronic infectious diseases, physical and chemical irritants);
- possible therapy.
Scleroderma diagnosis
The diagnosis is made based on the clinical picture. In doubtful cases, to clarify the diagnosis, a biopsy (examination of a piece of skin) is prescribed, followed by histological examination.
Since limited forms of scleroderma can sometimes transform into a systemic process, a laboratory examination is performed.
To exclude Lyme disease, a blood test is performed for tick-borne borreliosis.
Of great importance is a blood test for antinuclear antibodies, which are detected in 46-80% of patients and can serve as a sign of a more severe course of the disease, as well as the level of C-reactive protein and fibrinogen.
To identify concomitant diseases and contraindications to treatment, it is advisable to study a general and biochemical blood test, and a general urinalysis.
To exclude systemic scleroderma, consultation with a rheumatologist is required.
What is systemic scleroderma
What is scleroderma
Systemic scleroderma is a severe connective tissue disease in which the tissue thickens and hardens. The so-called sclerosis occurs (from the Greek sklerosis - hardening). Systemic scleroderma affects the skin, small vessels and internal organs: gastrointestinal tract, lungs, kidneys, heart. Women suffer from systemic scleroderma three times more often than men. The average age of patients is 30-40 years.
The cause of this disease is still unknown. Scientists suggest that congenital inferiority of the immune system, leading to autoimmune disorders, plays an important role in the development of systemic scleroderma. The human immune system suddenly begins to perceive its own cells as foreign and destroys them. In this case, connective tissue cells become its “enemies”. Risk factors for scleroderma include hypothermia, injury, and infection.
How does scleroderma occur?
Since systemic scleroderma affects various systems and organs, the manifestations of the disease are extremely diverse. Most often, the disease begins with the so-called Raynaud's syndrome (spasm of small blood vessels). At the same time, blood flow in the fingers is disrupted: they turn pale, become cold, and begin to hurt.
Skin changes also appear. In the early stages of the disease, edema (swelling) appears on the face and hands, which thickens over time. The color of the skin begins to resemble wax. The disease changes the patient's facial features: it becomes like a mask, and the mouth narrows. Due to the thickening of the skin, the fingers resemble a fake. Over time, the skin of the forearms, chest, neck, legs and feet is involved in the process.
In addition, symptoms of joint damage occur, manifested by pain and stiffness of movement. The gastrointestinal tract and heart are often affected. Patients complain of pain when swallowing food, constipation or diarrhea. They experience shortness of breath, arrhythmias, pain in the heart area, and swelling of the legs. Approximately 20% develop kidney damage.
Without treatment, the symptoms of the disease increase. In the acute form of the disease, the two-year survival rate does not exceed 20%; in the chronic form, about half of the patients live more than 5 years.
How is scleroderma diagnosed and treated?
If the symptoms described above appear, you should immediately contact a rheumatologist. Most likely, the doctor will make a diagnosis immediately after the examination, but in complex cases a biopsy of the joints and skin may be required. Sometimes patients are prescribed an immune test and a clinical blood test, which reveals general signs of inflammation. Heart changes are diagnosed using ECG and EchoCG (ultrasound examination of the heart). X-rays are used to detect changes in the lungs and joints.
For the treatment of systemic scleroderma, anti-inflammatory (corticosteroids), antifibrotic (preventing the compaction of connective tissue), vascular, immunosuppressive (suppressing the activity of the immune system) and restorative agents are used.
In chronic cases, balneotherapy (pine, radon and hydrogen sulfide baths), paraffin and mud applications, etc. are indicated. Physiotherapy, exercise therapy and massage are important. Based on materials from the article “Systemic scleroderma”.
Based on materials from the article “Systemic scleroderma”.
Causes of scleroderma
We talked earlier about the symptoms and causes of lupus erythematosus in women, but what are the causes of scleroderma?
At the moment, there are no reasons that fully explain the appearance of scleroderma in a patient. However, a number of factors have been identified that can provoke the occurrence of this disease (“trigger factors”).
Among them are:
- Past infectious and viral diseases;
- Impact of pregnancy and hormonal imbalance in women;
- Heredity;
- Complications after organ transplantation;
- Transfusion of blood components;
- Poor quality vaccines and serums.
In addition, factors such as hypothermia and prolonged exposure to stress can also lead to disruption of the normal functioning of the human immune system and the development of scleroderma.
New developments in the treatment of scleroderma
Medical scientists have long been studying the nature of scleroderma: what it is and how to treat this complex and serious disease. After all, traditional methods of therapy do not lead to complete elimination of the disease. New methods of treatment are being searched, drugs are being developed that can more effectively influence the pathology.
A new genetically engineered drug, Tocilizumab (Actemra), has been created. This drug is an antibody to interleukin-6 receptors. It is this anti-inflammatory cytokine that is the provoking factor in the occurrence of scleroderma and rheumatoid arthritis. Clinical studies have shown the effectiveness of the drug.
A new complex method of therapy with the enzyme “Lidase” in combination with vitamin preparations “Pantogam”, “Dexpanthenol” and “Picamilon” has been proposed. This method is effective for focal forms of the disease. Biologically active substances help improve metabolism in affected tissues.
Currently, research is being conducted on drugs that could block the signaling pathway for the development of scleroderma. Inhibitor molecules that can affect the pathogenesis of the disease are being investigated. This could help prevent fibrosis, an overgrowth of connective tissue. New developments in the treatment of scleroderma are also associated with the use of stem cells. They are able to replace diseased cells. This leads to a decrease in fibrosis and the formation of new blood vessels to replace those that were damaged by pathology.
Scleroderma signs, stages, varieties, photos (part 2)
Hello dear readers of my blog!
In a previous article, I talked about the basic concepts of systemic and focal scleroderma. We have discussed what focal and linear forms of the disease are. Now let's talk about rarer forms of scleroderma and its diagnosis.
Rarer clinical varieties of focal scleroderma include: macular (lichen sclerosus, white spot disease), Pasini-Pierini atrophoderma, deep, keloid-like and bullous scleroderma.
Treatment of scleroderma with medications
Treatment of scleroderma is carried out using the following groups of drugs:
- enzyme preparations;
- vasodilators;
- drugs that suppress the immune system;
- anti-inflammatory drugs;
- chelation therapy.
Treatment with enzyme preparations
The following drugs can be used:
- longidase;
- Ronidase;
- lidase;
- trypsin;
- chymotrypsin.
Treatment with vasodilators
The following vasodilator drugs are used in the treatment of scleroderma:
- Calcium channel blockers. Calcium channel blockers reduce spasm of vascular smooth muscle by reducing the supply of calcium, a mineral that is necessary for normal muscle fiber contraction. Verapamil tablets are used at a dose of 40–80 mg 3–4 times a day or nifedipine tablets at a dose of 10–20 mg 2 times a day.
- Phosphodiesterase inhibitors. Phosphodiesterase is an enzyme that is involved in the synthesis of a number of substances that can cause vascular contraction. These drugs have the greatest effect on the vessels of the pulmonary circulation, so they are used for pulmonary hypertension. Pentoxifylline is usually used at a dose of 600 mg per day.
Treatment with drugs that suppress the immune system
The following drugs are used to suppress the immune system:
- Cyclophosphamide is a drug that is widely used to treat many autoimmune diseases. Allows you to reduce the intensity of pulmonary fibrosis, slows down the formation of foci of sclerosis in the tissues of internal organs and skin.
- Methotrexate suppresses the division of immune cells in the blood, due to which it has a pronounced immunomodulatory effect. Research shows its high effectiveness against skin and lung lesions, as well as inflammation of muscles and joints.
- Cyclosporine inhibits the activity of T-lymphocytes, which play a key role in the development of diffuse scleroderma.
- Azathioprine suppresses the metabolism of substances that make up nucleic acids. Thanks to this, it blocks the process of cell division and reduces the intensity of the immune response.
- Rituximab is a drug that specifically blocks B lymphocytes responsible for the synthesis of antibodies.
toxic effects on the kidneys, bone marrow, heart, liver, reduce resistance to infections
Treatment with anti-inflammatory drugs
non-steroidal anti-inflammatory drugs swelling, pain, joint damage Non-steroidal anti-inflammatory drugs
| A drug | Mechanism of action | Mode of application |
| Diclofenac | Blocks the enzyme cyclooxygenase, which is involved in the breakdown of arachidonic acid at the site of inflammation to biologically active substances that have pro-inflammatory effects. Reducing the level of these substances eliminates the inflammatory reaction, swelling and pain. | Orally 75 - 150 mg in several doses, after meals with plenty of water. |
| Ibuprofen | Orally 800 mg 3 times a day after meals, with plenty of water. | |
| Meloxicam | Orally at a dose of 7.5–15 mg once a day after meals. | |
| Celecoxib | Orally in a daily dose of 200 mg in two doses. |
stomach gastritis ulcer meprazole, ranitidine, famotidine dexamethasone, prednisolone
Treatment
Treatment of systemic scleroderma is a lifelong process, and the regimen is always chosen individually
Experts take into account the course of the disease, the nature of the pathology, the form, and the degree of damage
It is extremely important for patients to follow all doctor’s recommendations and undergo regular examinations. The main objectives of the prescribed therapy are:
The main objectives of the prescribed therapy are:
- Prevention of vascular complications.
- Suppressing the progression of internal organ damage and skin fibrosis.
- Reducing activity and suppressing disease progression.
- Prevention and treatment of Raynaud's syndrome.
- Reducing swelling and tightness of the skin.
- Prevention of visceral manifestations of the disease.
To treat Raynaud's syndrome, it is recommended to wear warm clothes, avoid stressful situations or exposure to cold on the skin, and give up bad habits and drinking coffee. Factors provoking the disease reduce the effectiveness of treatment and lead to a slow but progressive pathology. One of the risk factors is ultraviolet radiation, which provokes an exacerbation of the disease. During periods of solar activity, you should avoid visiting open areas without special means to protect your skin.
Drug treatment
Taking medications is aimed at stabilizing the functional state and achieving the stage of remission, suppressing the activity of the process
It is also important to restore the function of internal organs, or prevent their damage if the disease is detected in the early stages. For this, the following types of drugs are prescribed:
Non-steroidal anti-inflammatory drugs (Ibuprofen, Piroxicam, Indomethacin). They are aimed at suppressing the inflammatory process in soft tissues, providing pain relief and improving the patient’s well-being. Vascular agents (“Foridon”, “Nifedipine”, “Corinfar”). These drugs block calcium channels, so they are widely prescribed at the initial stage of the disease. But they differ in effectiveness as the pathology progresses. Anti-inflammatory drugs (“Cuprenil”). They suppress the inflammatory process in tissues and have a pronounced antifibrotic effect. Prescribed for rapid progression of pathology
Prescribed with caution, as some types of drugs can have undesirable effects on the kidneys and intestines. Immunosuppressants (“Cyclophosphamide”, “Azathioprine”, “Methotrexate”)
They are effective against damage to muscles and joints, suppress the inflammatory process at the early stage of the disease, and slow down its progression. Glucocorticosteroids (Prednisolone, Dexamethasone, Metipred). They are prescribed in the later stages, during the acute course of the disease. But they definitely require constant monitoring of the condition of the kidneys, as they can have a negative effect on them. Enzyme agents (Ronidaza, Lidaza). Prescribed for chronic disease in the form of injections. Their peculiarity is to reduce the viscosity of hyaluronic acid.
The use of genetically engineered biological products is considered a new technique, but their effectiveness has not been proven today and is only at the study stage. This is a new direction in the treatment of systemic scleroderma. Such drugs include Inflixicamb and Etarnecept, but doctors prescribe them only as part of experimental treatment.
Changing your diet is an important part of treatment
Nutrition correction
Patients should definitely reconsider their diet not only for the period of taking medications, but also for the rest of their lives
It is important to design the menu in such a way that there are short intervals between meals and the portions are small. Foods high in protein are completely eliminated from the diet.
First of all, this applies to products such as:
- Fermented milk products.
- Seafood.
- Milk, kefir, fermented baked milk.
- Spicy cheese.
- Meat and fish.
- Products rich in calcium.
The presence of concomitant pathologies, such as renal failure, requires that food intake be strictly dosed, in compliance with a strict diet. Patients with systemic scleroderma are recommended to eat foods rich in vegetable oils and polyunsaturated acids, as they help suppress the inflammatory process in the body. Carbohydrates are consumed limited.
Scleroderma - symptoms
The clinical picture of the disease combines a complex of different signs that depend on the type of pathology. There are two main forms of scleroderma:
- Focal (localized)
- the disease affects individual organs and almost does not spread; it is easier to treat. - Systemic (generalized)
– a process affecting any structures containing collagen.
Focal scleroderma - symptoms
This variant of the pathology is more often diagnosed in children, and rarely occurs after 35-40 years. Localized scleroderma is divided into 2 types, both of which can be left untreated:
- Plaque or morphea.
The form of the disease in question appears as oval thickenings on the skin. The plaques are large and dense, white in the center, and purple along the edges. Visually it is easy to recognize that this is scleroderma; the photo below clearly reflects the specific symptoms. The disease sometimes goes away on its own, within 3-5 years, against the background of normalization of immune functions. In rare cases, pigmented spots remain in place of the plaques. - Linear scleroderma.
The presented variation of the disease is typical for young children. Banded areas with thickened epidermis form on the skin, mainly on the limbs and forehead. A feature of the linear form is considered to be unilateral damage to the body.
Systemic scleroderma - symptoms
The generalized type of pathology is also called progressive sclerosis of tissues and blood vessels. This is the most dangerous scleroderma; signs of the disease cover almost the entire body and are difficult to treat. According to the affected areas, the following forms of the disease are distinguished:
- Prescleroderma.
There are no visual symptoms, only Raynaud's syndrome is present - vascular spasms, accompanied by a feeling of coldness in the tips of the fingers, their pain and numbness. - Limited scleroderma.
This is a predominant lesion of the skin. With this type of pathology, internal organs undergo changes very slowly and after decades. - Diffuse scleroderma.
Rapidly progressive form. During the first year from the onset of the disease, blood vessels, skin, musculoskeletal system and internal organs are simultaneously damaged. It is difficult to treat. - Cross scleroderma.
A combination of the previous type of disease with polymyositis, vasculitis, rheumatism, dermatomyositis and other systemic pathologies. - Scleroderma without scleroderma.
Only internal and vascular symptoms occur; there are no skin manifestations.
Classic signs of pathology:
- Raynaud's syndrome;
- arthralgia;
- tenosynovitis;
- deformation of the nail phalanges;
- myopathies;
- polymyositis;
- heartburn;
- vomiting;
- ulcers and strictures of the esophagus;
- flatulence;
- diarrhea or constipation;
- reflux esophagitis;
- dysphagia;
- intestinal obstruction;
- cough;
- pneumofibrosis;
- expiratory shortness of breath;
- pericarditis;
- arrhythmia;
- thrombocytopenia;
- endocarditis;
- heart failure;
- polyneuropathy;
- autoimmune thyroiditis;
- biliary cirrhosis of the liver;
- Sjögren's syndrome;
- latent nephropathies;
- skin symptoms (shown in the photo below).
Focal scleroderma
The focal form of scleroderma is a local lesion of any area of the skin, which, as a rule, is not accompanied by significant systemic manifestations.
This variety is characterized by a relatively benign nature of the course and in some cases can disappear on its own. The affected areas in this form are a kind of “woody” skin compaction.
Typically, there are three stages in the formation of focal scleroderma:
- The stage of edema, in which characteristic purple-red lesions appear in the area of the skin lesion, resulting from an attack by the immune system and subsequent inflammation;
- The compaction stage, at which the lesions become denser, change their color to yellowish or white and subsequently become sclerotic (replaced by fibrin);
- Stage of atrophy , in which foci of hyperpigmentation and visible atrophy remain at the site of the affected area;
Due to the fact that areas of skin damage in focal scleroderma have different features and shapes, to facilitate diagnosis, it has been customary to classify it into the following subtypes:
- Plaque variety;
- Linear;
- Superficial
- White spot lesions (white spot disease)
Photo
Plaque focal scleroderma has the appearance of characteristic round (coin-shaped) skin changes. As a rule, they are single, dense, well demarcated from healthy skin and have a shiny surface. Such plaques are usually located on the extremities of the arms and legs, on the torso or face. Most often, this form of scleroderma affects women of reproductive age.
Photo
The linear variety has a peculiar appearance, which is also commonly called “saber mark”: an elongated spot with clear edges. Most often, linear scleroderma affects the scalp (both forehead and scalp), face, chest, and lower extremities. In addition, in some cases, this variety can form along the nerve trunks.
Photo
The superficial form also manifests itself in the form of plaques, however, they, unlike true plaque scleroderma, are loose, multiple and are not accompanied by significant atrophic lesions.
Photo
“White spot disease” is a separate form and has the appearance of multiple spots with a characteristic “porcelain” color and quite dense.
You might be interested! Vitiligo: what causes it and how to cure the disease?
As a rule, they affect the neck, upper half of the patient’s torso, genitals and even the oral cavity. The significance of this type of scleroderma is that it is often confused with another disease. Namely, lichen planus, which then leads to the prescription of incorrect treatment. Here you can read more about this disease and see photos of lichen planus.